We all like certainty; we like to think we know. That’s as true in psychotherapy as in any other field. We want to have faith that our current clinical approach is solid, that our treatments work well, that our particular kind of presence in the room is healing to a client. And that may be true—as far as we know.
But that’s the thing: we can know only so much at any particular moment in time. The future is the ultimate blank slate. We have no way of knowing what vital insight about emotional healing we’ve missed thus far, or what new approach might work better. The story of psychotherapy is a chronicle of this law of limited knowing—and of the recurring appearance of creative leaps that push us beyond our established understandings. To delve more deeply into our shape-shifting history, we’ve interviewed seven longtime leaders in a range of clinical specialties, asking them to tell the story of their particular realm as it’s evolved over four decades. These women and men were there, working in the trenches of their fields while alert to new possibilities. And so we asked them about it—about the original set of certitudes in their specialties, and what and who challenged them over the years, leading to the unfolding of fresh ways of thinking about, and doing, psychotherapy.
Change, of course, often breeds resistance. So our storytellers don’t flinch from describing the opposition that followed in the wake of new therapeutic ideas as well as the persistence and conviction of those who fought for possibly more powerful approaches. These oral historians reveal the ways in which our field has always been in ferment, powered by therapists who’ve noticed overlooked problems or elemental human needs that remained unaddressed—and then have tried to do something about it. While we hear about exhilarating eureka moments, our storytellers give equal time to mistakes and misdirections. In this way, we learn of the gritty, trial-and-error work required for meaningful new ideas to get the field’s attention and take hold.
The challenge each of our oral historians has faced has been finding a way to operate in two places at once—both inside the field as everyday clinicians, and outside it as critical thinkers, able to pull back and train a wider lens on the central question: how can we best support emotional growth and healing? These stories, at once social history and memoir, attest to how an openness to what doesn’t work creates a space for testing new ideas. This steadfast self-questioning is a big part of what makes this field as vital as it is.
Finally, these oral histories push us to ask ourselves: what might emerge next in psychotherapy? Might there be small refinements in our therapeutic approach, or even big leaps of faith, that are worth exploring? We can be sure that we have blind spots in our operating assumptions and methods, and plenty of alternative ways of serving as agents of change and growth that haven’t occurred to us. Not yet, anyway. There’s always so much to reimagine, to learn, and to do!
— Marian Sandmaier
Trauma
Retreats and Advances
by Bessel van der Kolk
Most people think the field of trauma treatment began around 1980, when the diagnosis of post-traumatic stress disorder (PTSD) was first included in the DSM as a result of a movement among Vietnam veterans. But one could actually go back well over a hundred years, to the work of Charcot and Pierre Janet at Salpêtrière in Paris. In fact, Janet in particular articulated most of the relevant issues about trauma that are being rediscovered today, such as getting stuck in reliving trauma, dissociating, and having trouble integrating new experiences and going on with one’s life. Janet primarily used hypnosis with hospitalized trauma patients to help them put the experience to rest, but his work was largely eclipsed by that of Sigmund Freud, in part because fully recognizing the devastating impact of trauma tends to be too overwhelming for mental health professionals and politicians alike. For example, Freud and his mentor, Joseph Breuer, wrote some outstanding papers on the nature of trauma in the 1890s, but they later repudiated them because suggesting the occurrence of incest in upstanding middle-class families in Vienna was so disturbing to their colleagues.
Ever since, trauma has had a history of cycling between being recognized for the devastating, long-term role it can play in people’s lives and then going underground in the face of resistance to that idea. The horror of trench warfare led to wide recognition of the symptoms of shellshock during World War I, but in 1917 the British general staff put out an edict forbidding the military to use the word shellshock to describe the condition, because they assumed it would undermine the troops’ morale. The same thing happened after World War II, when the world quickly forgot the price that we pay for sending young men (and now women) into combat. Yet all the symptoms that we read about in the newspaper—suicides, drug addictions, family violence, homelessness, and chronic unemployment—have been well documented after every war within modern memory, starting with the American Civil War.
Nevertheless, in the 1980s, as a result of the work of many people like Charles Figley—a Marine vet from Vietnam, who wrote a book called Trauma and Its Wake and started the International Society of Traumatic Stress Studies—trauma began to attract more and more attention in mainstream psychiatry and psychology. Around that time, Judith Herman and I began to study the relationship between borderline personality disorder and self-injurious behavior and early years of trauma and neglect at the hands of caregivers. However, in the early 1990s, just as had happened in 1902, 1917, and 1947, as the study of the trauma movement began to gather steam, there came a backlash.
In this case, it came in the form of the false memory movement, which tried to discredit the stories of abuse that our clients told us by calling them the result of therapists’ systematically implanting false memories in their minds. Much of this movement was fueled by the Roman Catholic Church as it was facing innumerable charges of priests’ sexual abuse of children, and by psychologists who could make a good living in forensic settings disputing the allegations by victims of sexual abuse. After the suits against the church were settled, the false memory industry disappeared with it.
One of the results of the controversy surrounding the false memory backlash was that the trauma field got bifurcated into two parallel areas of development, with basically all the research funding being directed to the military and veterans. The other area of research—child abuse and neglect and women’s studies—was underfunded and therefore unable to garner enough high-quality studies to determine scientifically how best to treat this population. As a result, our field became one of passionate claims, but little solid scientific evidence.
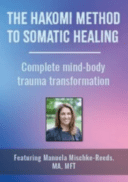
Nonetheless, some key developments (or, more precisely, in most cases, rediscoveries) have advanced trauma treatment. One has been the recognition of the role that dissociation plays in the aftermath of trauma and how, in various ways, treatment must address the personality structures that can compete or alternate with each other when someone is traumatized. Another major advance was the emergence of EMDR in the 1990s as the first approach that showed that we didn’t need to rely on drugs or the traditional talking cure to get traumatized people to leave their traumatic memories behind. Similarly, body psychotherapists have recognized that “the body keeps the score” when it comes to trauma and have revitalized bottom-up approaches like Somatic Experiencing, Hakomi, and sensorimotor psychotherapy to help shut-down people get unstuck from the fight/flight/freeze response.
Through neurofeedback, we’re exploring the capacity to rewire brains that are stuck in freeze and terror, and our first published studies of this process show how traumatized children and adults can learn to change how their brains regulate themselves. We’ve rediscovered that true change is best made when the mind is open. Mindfulness enables people to become attentive to their body and can enable them to feel safe. In fact, our NIMH-funded research shows that it looks as if yoga is more effective than any medication for treating PTSD.
Being able to be mindful is a necessary precondition for change. Hypnotherapists have long known that getting people into a trance state can facilitate the integration of trauma into their overall consciousness. More recently, Internal Family Systems and approaches that use mind-altering drugs like MDMA have demonstrated how to get people into altered states of consciousness where they can actually observe themselves and develop a sense of self-compassion that enables them to integrate their dissociated self from the past into in a calm state of mind in the present.
While all this has been going on, cognitive behavioral therapy (CBT) has accumulated the most research support, even though we know that the whole cognitive part of the brain shuts down when people are traumatized, triggering the primitive survival part of the brain. So using CBT with trauma is like telling somebody with an amputated leg to take up running. It can certainly give people a sense of perspective on their coping options when they’re in the right frame of mind, but it has limited value with severe trauma.
The most commonly used CBT approach to trauma is exposure therapy, which assumes that desensitizing someone to something that used to trigger them is the best way to help them be less affected by their memories. The problem is that desensitization leads to a global lack of feelings and engagement, so when you get desensitized from your trauma, you also get desensitized to joy, pleasure, engagement, and everything else going on. Desensitizing people shouldn’t be the goal of treatment: rather, we should help traumatized clients realize that Yes, this happened to me years ago, but not today; today is a different day, and I’m no longer the person I was back then. That kind of integration involves a neural network different from the neural network of desensitization.
My hope for the field of trauma treatment is that we learn how to help people bring their imaginations more fully to bear on their possibilities. For example, I’m involved with several theater programs for highly at-risk kids so they get to experience what it feels like to be somebody other than the identity that they’ve assumed. They can get the chance to say, “Oh, this is what it feels like to be a powerful general,” rather than “Nobody likes me; everybody hates me; I’m going to get hurt.”
I think theater and new techniques, like neurofeedback, can play an important role in calming the brain down and helping it become organized and more in touch with the body. In our culture, we too often rely on swigging alcohol and taking drugs to make ourselves feel better. Perhaps the most important contribution the therapy world, including the field of trauma, can make to the wider culture is to give people greater access to their innate self-regulatory systems—the way that they move, breathe, sing, interact with each other—so they can discover their natural resources to regulate themselves in a different way, especially when life gets challenging.
Couples
In Search of a Safe Haven
by John Gottman
The first book to have an impact on the field of couples therapy was The Mirages of Marriage by Don Jackson and William Lederer in 1968. Its basic premise was that the problem in distressed marriages was a failure of the implicit quid pro quo contract between partners when it comes to transactions around the exchange of rewards and positive feelings. The therapy approaches at the time focused on how to help people negotiate these contracts with each other from positions of self-interest, where each person was really trying to get the best deal for themselves as individuals. The role of the therapist was to be a kind of super-negotiator and problem-solver, the idea being that negotiating the best deals for each individual would result in the most satisfying relationship. And to sweeten things up, the authors encouraged couples to have “love days,” in which they did especially thoughtful things for one another.
Neil Jacobson and Gayla Margolin, psychologists at the University of Washington and University of Southern California respectively, were the ones who operationalized and researched this as a model of couples therapy in which people learned to be nicer to each other through contingency contracts, communicating better, and improving their conflict-resolution skills. But this approach had a fundamental theoretical flaw. Game theory—brought into psychology by Harold Kelley and John Thibaut—suggests that the only way you can get a really good contract is to work together with mutual trust. So each person needs to work not out of self-interest, but out of mutual interest, where the sum of the benefits is what the partners are maximizing. Otherwise, it becomes some sort of zero-sum game where it’s a win–lose paradigm. That was really the fundamental problem in those early days of behavioral marital therapy, the notion that you could work from positions of self-interest and still get a loving contract that really helps both people. It turns out that most of the time, people will sabotage that kind of a contract because it feels like an unacceptable compromise. And not surprisingly, when Jacobson analyzed the results of this approach to behavioral marital therapy, he found very small effect sizes and huge relapse rates.
The idea that transformed couples therapy emerged from attachment theory and the belief that what’s needed in marriage isn’t better contracts, but looking at marriage for a safe haven. That’s largely the contribution of Susan Johnson and Emotionally Focused Couples Therapy, which expanded John Bowlby’s idea about infants needing a secure base from which to explore their environment. Essentially, Johnson said that is what’s often missing in couples relationships, and she designed an approach to heal attachment injuries through extending Rogerian concepts of expressing emotions and paraphrasing and validating those emotions.
Beyond that, her big paradigm shift was bringing emotion into couples therapy. Before her, influential therapists like Murray Bowen had insisted that emotions got in the way of therapy. He famously said, “I don’t want to know what you feel; I want to know what you think.” The core concept in his theory of psychological differentiation was that at the highest level of development you could control your emotions with your reason. But then Johnson comes along and says, “No, that’s wrong: you really have to express emotions and validate them. Carl Rogers needs to be brought into the couples arena.”
So by focusing on emotion and the safe haven, Johnson wound up creating a revolution in couples therapy. And even though she wasn’t directly talking about trust, it’s essential in creating a safe haven, as is building commitment. The foremost researcher on commitment has been a woman named Caryl Rusbult, who came from social psychology, not from the psychotherapy tradition. Her 30-year research program is the only approach that’s ever been able to predict sexual infidelity successfully. All other research on sexual infidelity asks people to reconstruct from memory what happened before the act of betrayal occurred, but Rusbult can actually predict which couples will be sexually unfaithful.
She concluded that the basic element of betrayal is the tendency for partners to make negative comparisons. So when things get tough in a relationship, like you have an argument or your partner is emotionally distant, if you start to think, I can do better with someone else, you’re negatively comparing your partner to real or imagined alternatives. She found that when that happens, you’re going to invest less and less in the relationship and give yourself permission to cross boundaries and start relationships with other people. That’s where commitment comes in. People don’t recognize the enduring importance of a relationship very deeply if they have only a conditional investment in it. If you’re not really building gratitude by cherishing what you have with your partner, but instead are building resentment for what’s missing, you’re likelier to engage in an act of betrayal.
What the latest research from my lab is telling us is that trust and commitment are both the key ingredients for being in love with your partner for a lifetime, and for having your marriage be a safe haven. These are the ingredients for not just loving your partner, but being in love with your partner. And here the work of Helen Fisher is important. Fisher studies people who are in love. When she puts them in the functional MRI tube and they look at the face of the person they say they’re in love with (versus a stranger’s face), their entire pleasure center, the part of the brain that secretes dopamine, lights up. People used to say, “How long can you be in love with somebody? It’s got to have a shelf life of maybe 18 months.” Well, she’s found people who are still in love with their partner two decades after the wedding and longer. Apparently, being in love can last forever.
While Fisher’s work doesn’t focus on the ingredients that make that happen, I think future research is going to show that it’s based on building both trust and commitment. And we already have techniques now for doing that in couples therapy. The key element in making those techniques work is paying more attention to the moment-to-moment state of clients’ physiology. To do effective couples therapy, people really have to be calm when they talk to one another. And so the focus on conflict that pervaded couples therapy in its early years needs to be supplemented by calm, everyday emotional connection, where people can really talk to one another and listen and work on friendship.
Another thing we need to do is develop a system of shared meaning within the couple that has an existential base. When partners aren’t compromising in their essential conflicts, it’s because they feel as if the compromise means giving up a core part of themselves. Therefore, we have to get at the meaning of each person’s position in the conflict to resolve the majority of relationship conflicts. It’s also necessary to look at intentionally building shared meaning to have a connection that’s fulfilling and has some depth to it. It comes down to having a sense of shared purpose and meaning. For many couples, that includes a religious basis. William Doherty has been writing about this for decades.
Last, we need to look at the research that shows how unsuccessful most sex therapy is at evoking anything but the smallest changes. We’ve learned recently from a remarkable study—described in a book called The Normal Bar, which looked at 70,000 people’s sex lives in 24 countries—that the people who have a great sex life are doing about a dozen concrete things differently from those whose sex life sucks. It’s the same everywhere—in China, in Italy, in Canada, and in the United States—everywhere on the planet. The people who have a great sex life are saying “I love you” every day and meaning it. They’re kissing their partner passionately. They’re expressing affection in public. They’re cuddling. Research shows that only six percent of non-cuddlers have a great sex life. If couples don’t cuddle, they don’t secrete oxytocin, and their sex life isn’t fulfilling. It’s not rocket science.
Systems Therapy
The Art of Creating Uncertainty
by Salvador Minuchin
What became the family therapy movement began in the 1950s with a group of bright and curious individuals spread out across the country who were each fascinated in their own way in figuring out how families functioned. Initially, it actually had something of an antifamily attitude, emphasizing how families create pathology in their members, with Gregory Bateson and his group developing the concept of double-bind communication as a way of understanding how families can produce psychosis in children. There was also Murray Bowen at the National Institute of Mental Health talking about people being swallowed in the family’s undifferentiated ego mass. And there were others, like Carl Whitaker, Virginia Satir, and Nathan Ackerman. My own early work at the Wiltwyck School for Boys in New York looked at how the characteristics of families of the slums led to delinquency in children. It was only as we began to attract students who were interested in our work that we each encountered the need to conceptualize what we were doing more clearly and develop a coherent theory of practice that we could teach.
In 1975, when I wrote Families and Family Therapy, I thought that all therapists needed to do to translate their interest in understanding families into becoming effective therapists was to develop an alphabet of skills—how to join with families, do enactments, create boundaries, and so on. I believed that the poetry of therapy could be derived from this alphabet. But as I got more experience training therapists to use these techniques, it became clear that the techniques by themselves weren’t all that useful. It was therapists themselves who were the instruments of change, and to be effective, they had to recognize the way they were part of the system and the process in the therapy room, not just a neutral observer.
Unfortunately, the university training programs of today have shifted from a focus on the self of the therapist to what’s become known as core competencies. These competencies are concerned primarily with how to conceptualize cases and how to structure and engage in therapy sessions. Several competencies refer to the therapist’s awareness of the impact that the family is having on him, but overwhelmingly, trainees are expected to be thinking about what to do, rather than about who they are in the room with their clients. The best way I’ve found to understand this kind of self-awareness is to envision a therapist with a homunculus on her left shoulder, observing her mental processes and engaged in silent dialogues with her as she works.
All therapists need a range of tools to master their craft, but tools are just that—a means to accomplish an objective. When the carpenter begins with a piece of wood, he has an end goal in mind: to change that wood into something else. The saw, chisel, hammer, and nail are a means of transforming what the carpenter first sees into what he wants it to become. The effective family therapist also uses tools as means to an end, not as ends in themselves. The craft of family therapy lies in how these tools are used to produce a difference in the family—a useful change. An enactment on its own doesn’t move the family, but a therapist who understands that the enactment is a way to view the family’s interaction can shift the process. So the most important tool is the therapist’s use of self in guiding the process of change—and understanding how to use that tool is the biggest obstacle for beginning therapists. Ultimately, learning how to use the silent dialogue with the homunculus on one’s shoulder is central to mastering the craft of family therapy.
Besides my understanding of the craft of therapy, the related ideas of belonging and having multiple selves became more and more important in my work over the years. The systems that you belong to—that give you a sense of who you are and make you feel accepted—are the entryway to the experience of multiple identities. I see this now so clearly, both in my work and in my own life. I grew up in a Jewish family in a small town in Argentina that was a kind of shtetl where, up until the age of 12, I didn’t know anybody who wasn’t Jewish. Then at 18, I went to medical school, and my world grew larger. At 20, I was put in jail for three months with a group of other students for protesting against Perón, and my concept of myself changed again: I became an Argentinian Jew who was committed to social justice. From then on, I was a revolutionary and a fighter for social justice, and it seemed natural that I should join the Israeli army, in which I served as a doctor during the War for Independence. Later, when I emigrated to the United States and was on the staff at the Wiltwyck School for Boys, I was a cultural outsider and found myself identifying with the poor black people around me as I learned to speak English. And as I came to feel that I belonged with the staff and children and families at Wiltwyck, I felt I expanded even more.
My idea that we’re all multiple selves led me to develop a therapy of challenge, rather than one of being gentle with people. My goal as a therapist wasn’t to be cautious and empathic, but to be an intervenor who creates uncertainty in clients about who they were and are and what they’re capable of becoming. I wasn’t interested in their “true self”: I wanted them to experience a series of selves and the expansion of possibility that can grow from that experience. Above all, I wanted them to recognize that there were more ways of being than what their life experience so far, whatever it was, had made them aware of. What I did in therapy was say to people, “You know, belonging may give you a sense of security, protection, harmony, but it also limits you and creates an invisible pattern of relationship that fools you into believing it’s the only way of being.”
So when I look back on my life, I see a sheltered Jewish child, a rebellious young adult, a revolutionary, a soldier, a stammering, helpless immigrant, and many, many, other things. At 95, I think of myself as having journeyed through life as many different people, and I think of a line from Antonio Machado, one of my favorite Spanish poets: “The road is not the road; you make the road by walking.” I hope in my own walking I’ve cleared away some debris for those who will follow.
Family Violence
Out of the Shadows
by Mary Jo Barrett
Just before I began graduate school in 1974, the Child Abuse Prevention and Treatment Act was enacted—the first authorization of federal funds to improve the states’ response to physical abuse, neglect, and sexual abuse in families. Before then, in many states, if you suspected a child or a woman was the victim of domestic violence, it was unclear whom you were supposed to contact. In some places, you actually called the Humane Society or, more likely, the police. The idea was, “Don’t get involved in other people’s families. It’s too messy.” Women and children were still looked at as property. But by the time I got my first job as a contractual in-home therapist for the Department of Children and Family Services in Illinois in the late ’70s, my agency was being inundated with phone calls, and my supervisor admitted to me, “We don’t know what to do with all these cases.”
Back then, when professionals in the child welfare world were just beginning to consider the idea of therapy for abuse and neglect, the typical course of action was a “parentectomy”—taking children away from their parents and putting them in foster care, without ever dealing with what had been going on in the original family. That practice evolved into the idea of finding the least restrictive environment possible—meaning a placement, usually with a family friend or relative, where children wouldn’t experience the removal from parents as a punishment or an indication that they’d done something wrong. But in the mid-’80s, as it became clearer how disruptive removing children from their homes could be, a family-preservation movement emerged, devoted to keeping children with their parents if possible. It recognized that children not only didn’t thrive in foster care, but were often abused and neglected there all over again.
A tenet of the family-preservation movement was the goal of getting the foster parents and biological parents to work together. Much of that work took place in the home, not in an office or agency. The model emphasized keeping the biological parents involved, rather than cutting them off, and helping them stabilize and learn new parenting skills. Working with this population, I spent much of my time in homes talking with parents about the ordinary problems of everyday life, discussing subjects like nutrition and even helping them clean out their refrigerators.
When I’d check in with my consultant, Carl Whitaker, he’d remind me how crucial it was to be in the home at the times when a frustrated parent might lunge at a misbehaving child; such times would give me opportunities to turn angry episodes into teachable moments. One mom and I would watch the soap opera All My Children each week together and talk about how the women in an episode were being treated or who she thought was a good mother. The discussion always led to her own life and how I could help her change. Whitaker taught me not to turn off the television, but to utilize it within my therapeutic work.
Of course, we know that family violence involves a web of factors that contribute to the abuse. But in the ’70s and ’80s, many feminists championed a more linear view of abuse, emphasizing the role of male privilege and patriarchy, and the importance of separating perpetrators of violence from their victims. I remember being in the middle of a workshop on family violence, incest, and domestic abuse in the early ’80s, when I heard loud noises in the hall. Some therapists were passing around flyers, yelling that my approach in seeking to help families stay together was dangerous to women and children—and that I was “in bed with perpetrators.” At that time, very few programs treated offenders of any type, and virtually none integrated individual and family therapy for offenders as well as victims.
This was a time when incest and child sexual abuse were still taboo subjects. The conventional wisdom was that they occurred only rarely. Then we began to wake up. Diana Russell, in her 1984 book Sexual Exploitation, reported that 16 percent of women had been sexually abused by a relative before the age of 18, and 31 percent had had at least one experience of sexual abuse by a nonfamily member before that age. Researcher David Finkelhor published A Sourcebook on Child Sexual Abuse soon after, reporting that nearly 20 percent of college woman and nearly 9 percent of college men had been sexually abused before the age of 18 by someone they knew.
Around this time, Laura Davis and Ellen Bass, a survivor and her therapist, published The Courage to Heal, addressing the question of what sexually abused women needed to do to recover. The book was a powerful call to action, urging abuse victims to trust their instincts about dark memories of childhood abuse, confront their alleged abusers, take pride in their identity as a survivors, and find therapists to help them recover memories of abuse that were often shrouded in uncertainty. The Courage to Heal gave many people permission to speak about something that had been previously unspeakable, opening the door to a public discussion of a previously off-limits subject.
But while The Courage to Heal empowered survivors to voice their experiences, most therapists had little to no training in addressing family violence. So many of them floundered in the dark with this new type of client, inventing and adopting techniques that weren’t grounded in research or accepted therapeutic practices. They rebirthed clients on the floor of their offices, or used hypnosis to retrieve memories. They sometimes coached their clients to write angry letters to their parents, or to confront them in person. The result was often irresponsible therapy, which cast the clients as defenseless victims and therapists as rescuers. Some therapist even suggested to clients that they write letters to people’s employers, warning them that a sexual offender was in their midst. And survivors were sometimes encouraged to inform their siblings that they too must be repressing incidents of abuse.
Then, with the advent of the false memory movement of the early ’90s, it all exploded. Groups of parents whose children had confronted them about child abuse began to fight back. Many filed lawsuits against therapists for implanting memories and turning their children against them. Aggrieved parents and their supporters protested outside therapists’ offices. They heckled speakers at conferences where therapists were trying to learn more effective ways to deal with child sexual abuse. Instead of recognizing how scared and threatened accused parents were and finding creative ways to include the family in a healing process, frightened therapists just began to tell clients, “I don’t want to talk about your sexual abuse history.”
This backlash undercut the development of effective treatment approaches to family violence. It also discouraged clinicians from including family members in therapy, forcing them to shy away from more inclusive, systemic approaches and focus narrowly on individual survivors and their trauma history. In my view, even today, one of the biggest obstacles to the effective treatment of family violence is facing the challenge of involving the offender in treatment, as well as the rest of the family. We must recognize that abuse is more than a power imbalance of parents over children or men over women: it involves the attachment wounds that underlie acts of abuse and neglect, especially the panic that comes from feeling both powerless and disconnected in an intimate relationship.
Family violence remains a national health problem that few therapists have been trained to deal with and, sadly, few of us want to address. On a good day, it’s a messy, complicated business, which doesn’t bring much financial reward or professional status. We still haven’t found a way to apply the emotional/spiritual/neuropsychological approaches to healing that have been integrated into our models of other types of family issues. And we continue to neglect the child welfare world—the parents who are reliving their own trauma through the abuse and neglect of their own children, not to mention the men and women for whom being abused is a daily experience. Underfunded and undertrained, the clinicians who work with these clients rarely receive much attention.
Unfortunately, the new political climate is likely to make the victims of family violence feel even more powerless, out of control, and devalued. But though we started out in the ’70s not knowing what to do with these clients, we now have a lot more knowledge of how to help them. All we need is the will and commitment to apply what we’ve learned to treating this vast and underserved treatment population.
Psychopharmacology
The Jury Is Still Out
by John Preston
Even though lithium was around in the late 1940s, psychopharmaceuticals really began to reshape mental health treatment in the 1950s, when the first antidepressants, tranquilizers, and antipsychotic medications were discovered, mostly through attempts to treat other kinds of illnesses and accidentally finding that some drugs had an effect on psychiatric conditions. These meds were light-years ahead of treatments that had existed before, but they had a lot of side effects, especially the tricyclics and MAO inhibitors, which were really toxic if taken in overdoses. You could take a handful of Elavil, for example, and kill yourself.
The big breakthrough came in 1987, when Prozac, Paxil, and Zoloft came on the market. The major feature of this new generation of antidepressants was that they weren’t as toxic. You could take a bucket of Prozac, and it wouldn’t kill you. You might have the worst diarrhea of your life, but pharmaceutical companies didn’t have to worry about being sued over people using their product to commit suicide. In effect, this led companies to push these meds not just to psychiatrists, but to primary care doctors. So in the next five years, the stats show a fourfold increase in prescriptions for antidepressant medications from primary care doctors.
That began a revolution that changed the landscape of the mental health field over the next three decades. In 1998, 74 percent of depressed clients were being treated with antidepressants, and 75 percent were being treated with psychotherapy; but by 2016, 75 percent of people receiving treatment for depression were on meds, and only 43 percent were in psychotherapy. All this was happening at a time when the psychotherapies for things like depression and anxiety disorders were getting better and better.
The pharmaceutical companies— even though they didn’t have the research to show that the drugs were actually more effective than psychotherapy—watched Prozac become one of the most popular drugs ever, making billions of dollars, and they realized they had a gold mine. Then managed care and HMOs took advantage of this, because sending people to primary care doctors costs them a lot less money than sending people to psychiatrists. Not surprisingly, however, studies show that the outcomes for people treated for depression by primary care physicians are very poor. Furthermore, most primary care doctors don’t refer people for psychotherapy. So while this is a cost-saving solution for managed care, it hasn’t been good for the overall quality of mental health treatment and psychotherapists’ livelihoods. Today, about 85 percent of drug prescriptions for anxiety and depression come from primary care doctors.
The SSRIs were touted as user-friendly drugs, but over time, unwanted side effects have become apparent. All the antidepressants except Wellbutrin have significant effects on serotonin and can cause sexual side effects. About 25 to 30 percent of people on SSRIs complain that while they maintain the capacity to get aroused, they can’t easily have an orgasm, which causes many of them to stop taking the medication. A side effect of taking SSRIs long-term that’s even more concerning and hasn’t gotten enough attention is the blunting of affect. It usually doesn’t happen right away, and it’s so gradual that sometimes people can’t tell what’s happening until they wake up one morning and say, “You know, I just don’t feel good.”
Two things are going on here. One is apathy, just not having a sense of energy to get up and do stuff or get excited about things. The other is feeling emotionally numbed out. This is underscored by an inability to cry, which is obviously an important and healthy human emotion. In a New Zealand study, 24 percent of the people who responded well to an antidepressant with reduced suicidal ideas and depressive symptoms said they felt numbed out, and another 36 percent said they felt severely blunted. In effect, more than half were saying, “I’m grateful I can get out of bed every morning, but although I’m not going to kill myself, I just don’t feel like myself.”
In the early ’90s, another major wave of drugs became ascendant among prescribers. These were the second-generation or newer antipsychotic medications. They were popular because they were much less likely to cause severe problems like tardive dyskinesia and Parkinsonian symptoms, and they were especially good for treating schizophrenia as well as acute mania. But over time it emerged that at least half of them could create metabolic symptoms, changes in blood glucose levels, increased rates of diabetes, and increased cholesterol and triglycerides. It doesn’t happen within weeks or months, but the long-term increase in heart attacks and strokes is a serious problem.
More recently, psychotherapists, especially in Europe and Canada, have made big strides in integrative treatments, which include bright-light therapy and circadian stabilization, as some people now say that mood disorders are in part a disorder of circadian rhythm. There’s also been more interest in diet and nutritional approaches, which include taking folic acid and omega-3 fatty acids, as well as exercise.
This comes at a time when evidence is increasing that conditions like panic disorder, OCD, generalized anxiety, and social anxiety are really chronic conditions that don’t just get better over time: they’re lifelong disorders that ebb and flow. We have good drugs for them, but when most people stop taking them, the symptoms return. Psychotherapeutic approaches, especially CBT and exposure therapy, show better outcomes, but they require the client to do a lot of homework and hang in with exposure work that can be difficult. Still, the results for more than 80 percent of those who complete treatment can be more or less permanent. Despite all this, psychiatrists almost exclusively promote the use of medications, while nonmedical practitioners typically advocate treatments that don’t involve drugs. This is an ongoing polarization within the field.
Another issue that’s gone largely unrecognized and will profoundly affect the future of mental health treatment is that fewer and fewer medical students are signing up for psychiatry as their specialty. Over the last 20 years, their number has dropped by 50 percent. Currently, about half the psychiatrists in the United States are over 60—which means they’re on the cusp of retirement—while more primary care doctors are prescribing meds. Young physicians, it seems, aren’t interested in going into psychiatry because it doesn’t pay as much as other specialties, and all you’re doing is giving out pills. I know two psychiatrists who started their career using medicine and doing psychotherapy, but now the only thing they get reimbursed for is handing out drugs.
As for new approaches in psychopharmacology, a couple of interesting developments are focusing on finding neurochemical targets in the brain that are different from those used by current meds. The drug that’s probably gotten the most attention is the anesthetic ketamine, given in very low intravenous doses. For some people, it seems to have a remarkable, fast-acting effect on extremely severe depression. It doesn’t target serotonin or norepinephrine at all, the usual suspects in drug treatment. Instead, it targets the neurotransmitter glutamate. Although the issue of side effects, especially liver problems, is a source of concern, people are excited about the prospect of finding the holy grail for treating anxiety and depressive disorders with a drug that works within hours.
One last thing that’s looking promising is the recent finding that up to a fifth of people who have chronic or recurring depression may have underlying chronic inflammation. When they’re treated with large doses of anti-inflammatories, the depression goes away. This is absolutely experimental, but I think the cutting edge of psychopharmacology this year will be inflammation.
Ultimately, while psychiatric drugs do save lives, the fact remains that integrative treatment (psychotherapy, lifestyle changes, exercise, and sometimes medications) works best. It behooves us to give our clients the best we have to offer, which involves much more than just offering pills to temporarily relieve symptoms. While the economics of mental healthcare keep oversimplifying treatment and emphasizing the power of the magical pill, research continues to show that the most effective approaches pull out all the stops and tackle mental illness on multiple levels.
Race Matters
How Far Have We Come?
by Kenneth Hardy
In the late 1970s, I was a black kid from Philadelphia enrolled in the family therapy graduate program at Florida State, an institution that had graduated its first black grad student only in the mid-’60s. I was the only black student in the program, and there were no black faculty. Issues of race as a factor in people’s lives rarely came up in class. If I brought it up with my supervisors, they responded, “If you want to be a good clinician, just learn the rudiments of family therapy and then apply them to whatever family you see. Don’t make race a special issue.” The entire emphasis was about generalized treatment methods without paying attention to race, class, or gender issues.
Then, through the early 1980s, the feminist critique began to expose the rampant gender-based inequities and sexism inherent in the field and the way family therapy perpetuated mother-blaming in its explanation of family interactional patterns. It made what had been previously invisible impossible to ignore. Nevertheless, largely advanced by white women, it didn’t directly address issues of racial inequality and racism, even though by pointing out how family therapy privileged males, it also exposed the privilege enjoyed by white people. Just like women, people of color were marginalized. Seeing how the field’s feminist leaders pushed boundaries and withstood the firestorm of criticism they received from the influential men in the field was both inspiring and a little frightening for therapists of color. I remember thinking that if whites could so viciously attack each other over their differences about gender issues, what would happen to people of color who dared talk openly about race and racism.
One moment at an American Association of Marriage and Family Therapists (AAMFT) national conference in 1984 stands out for me as especially powerful. Feminist therapist Marianne Walters, in her keynote address, called attention to both the issues of sexism and racism by flashing on a big screen the pictures of all the keynote speakers and members of the AAMFT board of directors. She began by saying that she wanted to pay homage to the thinkers and shapers of the field, and then one by one, she thanked them by name. As images of one white male after another loomed over the ballroom, the extent of the overwhelming gender imbalance among leadership roles became more and more apparent. So albeit in a somewhat indirect way, the feminist critique drew attention to racial privilege as well.
During this period, there were certain books that succeeded in raising consciousness about social issues within the field. Although Monica McGoldrick’s groundbreaking Ethnicity and Family Therapy didn’t deal with race specifically, it succeeded in adding ethnicity and culture to the list of contextual factors that should be considered when working with families. Unlike the feminist critique, the topic of ethnicity was easy for everyone to discuss, because it didn’t call attention to structural inequities, power, and privilege. Even more importantly, Nancy Boyd Franklin’s book Black Families in Therapy marked a crucial milestone for the field by focusing on the special challenges black families face in a racist society. And it was practical to boot, providing tips and tools for effectively engaging and treating black families.
Nevertheless, it was still hard to get material about race into academic journals because reviewers found it too inflammatory. I remember conference organizers discouraging me from focusing directly on race in my talks and strongly encouraging me to instead use the less threatening term multiculturalism. After all, the major power brokers of the field at the time were white: all the editors of family therapy journals (a fact that remains true today), all the officers of the major family therapy organizations, the plenary speakers, the field’s most charismatic gurus. For people of color, forcing a conversation about race seemed like committing professional suicide. So some of us took a more strategic approach. I remember publishing a paper called “The Theoretical Myth of Sameness: A Critical Issue in Family Therapy Treatment and Training” as a safe way to examine the potentially explosive issue of race in a more general discussion about “sameness and difference.” I was opening a door without sounding too confrontational.
In the climate of the times, even giving a workshop explicitly on race and racism seemed like a big step forward. One year, I offered a session called “Breaking the Silence” that gave voice to the sense of stifling frustration, deep disappointment, and race-related pain that many people of color felt unable to openly express to their white colleagues. For people in the minority community, it was as close to an open act of defiance as many of us had come: no more walking on eggshells regarding issues of race, no more apologies for acknowledging when and how we saw racism in the field. For my own part, I’d learned a lesson or two from my feminist friends about the courage it took to be outspoken about “divisive issues,” and the importance of taking good care of yourself in the face of the inevitable pushback that comes from pointing out differences in power and privilege that are built not only into society, but the mental health profession as well.
Throughout the 1990s, my process of becoming more transparent about the struggles of being a black therapist in the field continued. I published an article in the Networker called “War of the Worlds,” in which I talked openly for the first time about the compromises people of color in the field have to make to be deemed acceptable by their white counterparts. To date, nothing I’ve written for the Networker, or any other publication, has generated more personal letters—strongly supportive as well as scathingly critical—than this one. Then in 1996, I gave a keynote at the Networker Symposium. It was the first time that a nonwhite clinician had delivered a major plenary address at a national family therapy meeting of such a size.
Pleased as I was to receive the invitation, I also felt the tremendous burden of responsibility as I began my talk extemporaneously by describing all the voices of black people for whom I felt I was a representative. It was a very emotional experience for me. Designed to engage the broadest possible audience, my theme was the sense of “psychological homelessness” that so many people of color struggle with as they try to fit into different, mutually exclusive worlds, leaving them without a safe place, a true home. Women, gays and lesbians, immigrants, estranged daughters and sons, and emotionally cut-off parents could all relate to what I was saying as a black person about the depth of my need to feel safe, valued, and connected to others. In the years that followed, it was gratifying to start seeing other people of color become more prominent at those kinds of forums.
By the late ’90s, an increasing number of training programs began developing curricula that specifically addressed issues of race and social justice. This was instrumental in attracting more trainees of color to family therapy programs. The Couple and Family Therapy Program at Drexel University in Philadelphia has been a leader in graduating a large number of family therapists of color. The Ackerman Institute for the Family in New York City developed a minority social-work program. Monica McGoldrick’s Multicultural Family Institute in New Jersey and Nancy Boyd Franklin’s Psychology Program at Rutgers University in New Jersey have also produced a large group of skilled therapists of color over the years.
But while there’s been a positive shift in our awareness of race, the discomfort and awkwardness in addressing it is still prevalent. Regardless of the venue or the participants, conversations about race are difficult to facilitate. People of color fear being judged as race-obsessed, angry, and hypersensitive. And whites often fear being misunderstood, perceived as a racist, or saying something that will trigger the anger of people of color. For the most part, a fundamental attitude of mutual mistrust underlies discussions of race between blacks and whites, making meaningful interactions across the great divide of race hard to achieve. It takes both will and skill to address the issue of race, and even though the will has generally increased, the skill is still lagging behind.
Over the years that I’ve been facilitating these kinds of interactions, I’ve realized that the most successful ones must start with the soul work of seeing, being, and doing. Seeing is about our increasing ability to recognize how much the color of our skin defines our day-to-day experience. The next step is being able to engage in a process of self-awareness about what it means to be white or a person of color and what role we choose to play in addressing the racial inequities we see around us. The final step is, of course, the most difficult—to actively engage in doing something about them.
If ever there were a critical moment for constructive and courageous conversations about race, power, and privilege in our practices, communities, and the broader society, this is it. Personally, I feel affirmed in the credo that whatever our training or orientation, our work as clinicians should ultimately be devoted to healing the world, even if it means addressing that huge task in 50-minute intervals at a time.
Neuroscience and Therapy
The Craft of Rewiring the Brain
By Daniel Siegel
In 1978, when the Psychotherapy Networker was born, I was just beginning medical school. Back then, little was known about the workings of the living, dynamic brain, but by the mid-’80s, technology in the form of CAT scans and MRIs enabled us to see some aspects of neural structure and function inside our previously opaque skull. Still, as I started my training, first in pediatrics and then in adult, adolescent, and child psychiatry, I struggled to find a way to combine my fascination with science with what I was learning as a psychotherapy student. What I sampled from the smorgasbord of therapeutic modalities—from family and couples therapy to psychodynamic methods and cognitive-behavioral approaches—seemed to inhabit a world separate from important developments in the broader scientific community—in fields like neurobiology, child development, evolutionary psychology, cognitive science, anthropology, sociology—that might advance the craft of psychotherapy.
At that time, we were taught that the brain was fully formed by adulthood. But if this were true, what in the world could we do as psychotherapists that might lead to lasting changes in our clients’ brains? The orthodox teaching in neurobiology also asserted that certain regions “gave rise” to specific mental functions, like memory, mood, and language. If this were true, then a malfunctioning mind was due to dysfunction in a particular region—and short of giving a pill, what could a therapist do to improve that region’s functioning? Luckily, these two axioms would soon be overthrown, as we learned that the brain responds to experience throughout the lifespan by changing its function and structure, and that you could look to the connections of regions—and grow those connections—to understand how to move clients from dysfunction to function, even in adulthood.
But yet another obstacle was getting in the way of our recognizing the fresh possibilities that were opening up. We still believed in something Hippocrates had asserted 2,500 years ago: the “mind is what the brain does.” Could our mental lives—our emotions, thoughts, memories, and meaning-making narratives—be nothing more than simply neurons firing off in our head? If our mind was only a brain, we were left with a self-contained, single-skull view of mental life—which implied that our relationship with others, all the richness of human connection, was superfluous to mental functioning. Deep down, unsupported by much scientific evidence to the contrary, many therapists sensed that this simply couldn’t be the whole story of the mind.
Then came the 1990s—“The Decade of the Brain,” as dubbed by President George H. W. Bush—which brought us a new perspective on the brain as self-renewing, with capacities to rewire itself in response to changing circumstances. This went well beyond old assumptions about our innate, hardwired limitations. New findings about neuroplasticity took us beyond anecdotes and metaphors and vague theories into a more measurable science of human nature, incorporating both the biological and the personal.
For me, one of the first steps in a new, science-based view of psychotherapy came with the work on attachment theory by people like John Bowlby, Mary Ainsworth, and Mary Main. Together, the different threads of their work not only showed how early experiences shape our personalities, but in a finding with vast implications for psychotherapy, revealed the central importance of a coherent narrative in people’s grasp of their own lives. Mary Main showed how if adults could create reflective, coherent, and emotionally rich narratives about their childhoods, their own children were likely to form a good, secure relationship with them, no matter what type of attachment they themselves had had when growing up. It wasn’t what had happened to them as children, but how they’d come to make sense of what had happened to them that predicted their emotional availability as adults and the kind of parents they’d be.
An equally important discovery with powerful implications for psychotherapy was the discovery of the role of the horn-shaped hippocampus and how it created the difference between implicit and explicit memory. Implicit memory is a form of emotional, sensory, or behavioral memory that doesn’t include recalled facts or place inner experience on a timeline from the past. Trauma can flood the amygdala to create intense implicit memories but shut off the hippocampus so that the horrible sensations of life-threatening events are blocked from becoming explicit memories. That’s why people with PTSD experience their memories in the here and now, without having the sensation of remembering them. They find themselves overwhelmed by the retrieval of powerful sensations drawn from pure implicit memory that lacks a sense of something coming from the past. This process makes PTSD survivors vulnerable to flashbacks and dissociation. It also reveals how distinguishing a past memory from present life can enable clients to move forward into the future without the fear that the past will continue to haunt them. The key is the neural integration between differentiated areas of the brain, allowing the past event to become no more and no less than an aspect of an autobiographical story that makes sense of life.
By the mid-’90s, together with a group of colleagues at UCLA from a range of scientific disciplines, I began to explore the relationship between the mind and the brain. Along with others in clinical fields, we explored ways that integrating brain functions might be therapeutically beneficial for clients, especially those who had an impoverished sense of their own past and couldn’t really feel or express emotion. We found that lots of clients who usually intellectualized their way through talk therapy responded well to guided imagery, sensate body focusing, and practice in using and picking up on nonverbal cues. Inspired by the work being done on neuroplasticity, we began to look at how therapy can catalyze neural growth to create long-lasting change. Could it be that the way you think can actually change your brain?
In the first decade of the new millennium, interest in mindfulness was beginning to burgeon in the field, offering new evidence, now measurable through advances in technology, that the way we focus attention within awareness can change our brain. Neural firing changes neural connection, and if we intentionally pay attention, this can transform the very structure of the brain. Mindfulness, we learned, promotes the integrative function of the various regions of the brain, including the prefrontal cortex. It allows brain circuits to fire together that perhaps have never fired in this coordinated way before, giving people a sensation of inner awareness that they may never have had. It can open the pathway to neural integration—the linkage of different parts of the brain—and enhance powers of self-regulation.
Almost every mental health problem—anxiety, depression, eating disorders, personality disorders, thinking disorders—are issues of self-regulation. Ultimately, the goal of therapy is to optimize self-regulation, the coordinated flow of energy and information through the major systems of the brain—brain stem, limbic circuits neocortex, autonomic nervous—and then between one brain and another. When we’re in this secure, stable state of mind-brain-body equilibrium, we can face life’s vicissitudes with some measure of emotionally calm flexibility, self-awareness, and reason.
As we broaden our appreciation of what science can teach us about the complexity of human functioning, it becomes clear that clinicians serve as transformative attachment experts, whose job it is, in effect, to help rewire unintegrated neural connections, to reintegrate (or sometimes integrate for the first time) different areas and functions of the brain—implicit and explicit memory, right and left hemisphere, neocortex with limbic system and brain stem.
The past 40 years have given us a view of the mind that encompasses an emergent, self-organizing, embodied, and relational process that regulates the flow of energy and information. We now know that where attention goes, neural firing flows, and neural connection grows. We’re finally equipped to embrace the wide array of sciences to see the myriad ways therapy can focus attention to stimulate the coordination and balance of neural firing that leads to the growth of neural integration and optimal health.
Helping people develop more integration goes beyond reducing symptoms: it helps them thrive. And integration also has its moral dimensions, pointing us in the direction of being kind and compassionate to ourselves and others. So now, more than ever, we as mental health practitioners need to be aware of the crucial importance of integration in human functioning and find ways to harness the power of psychotherapy to create a kinder, more compassionate, and integrated world.
Illustration © Nicholas Wilton
Marian Sandmaier
Marian Sandmaier is the author of two nonfiction books, Original Kin: The Search for Connection Among Adult Sisters and Brothers (Dutton-Penguin) and The Invisible Alcoholics: Women and Alcohol Abuse in America (McGraw-Hill). She is Features Editor at Psychotherapy Networker and has written for the New York Times Book Review, the Washington Post, and other publications. Sandmaier has discussed her work on the Oprah Winfrey Show, the Today Show, and NPR’s “All Things Considered” and “Fresh Air.” On several occasions, she has received recognition from the American Society of Journalists and Authors for magazine articles on psychology and behavior. Most recently, she won the ASJA first-person essay award for her article “Hanging Out with Dick Van Dyke” on her inconvenient attack of shyness while interviewing. You can learn more about her work at www.mariansandmaier.net.
Bessel van der Kolk
Bessel A. Van der Kolk, M.D., is a clinician, researcher and teacher in the area of post-traumatic stress. His work integrates developmental, neurobiological, psychodynamic and interpersonal aspects of the impact of trauma and its treatment. Dr. van der Kolk and his various collaborators have published extensively on the impact of trauma on development, such as dissociative problems, borderline personality and self-mutilation, cognitive development, memory, and the psychobiology of trauma. He has published over 150 peer reviewed scientific articles on such diverse topics as neuroimaging, self-injury, memory, neurofeedback, Developmental Trauma, yoga, theater and EMDR.
He is founder of the Trauma Center in Brookline, Massachusetts and president of the Trauma Research Foundation, which promotes clinical, scientific and educational projects. His 2014 #1 New York Times best seller, The Body Keeps the Score: Brain, Mind, and Body in the Treatment of Trauma, transforms our understanding of traumatic stress, revealing how it literally rearranges the brain’s wiring – specifically areas dedicated to pleasure, engagement, control, and trust. He shows how these areas can be reactivated through innovative treatments including neurofeedback, somatically based therapies, EMDR, psychodrama, play, yoga, and other therapies.
Dan Siegel
Longtime Psychotherapy Networker contributor Daniel J. Siegel, MD, is a graduate of Harvard Medical School and completed his postgraduate medical education at UCLA with training in pediatrics and child, adolescent, and adult psychiatry. He is currently a clinical professor of psychiatry at the UCLA School of Medicine, founding co-director of UCLA’s Mindful Awareness Research Center, founding co-investigator at the UCLA Center for Culture, Brain and Development, and executive director of the Mindsight Institute, an educational center devoted to promoting insight, compassion, and empathy in individuals, families, institutions, and communities. Dr. Siegel’s psychotherapy practice spans thirty years, and he has published extensively for the professional audience. He serves as the Founding Editor for the Norton Professional Series on Interpersonal Neurobiology which includes over 70 textbooks.
John Preston
John Preston, Psy.D., ABPP, is a professor with Alliant International University (California School of Professional Psychology), Sacramento. He has also taught at UC Davis, School of Medicine. He is the author/co-author of 21 books on various topics including depression, psychotherapy, psychopharmacology, borderline disorders, bipolar disorder, and post-traumatic stress disorder. He is the author of “Drugs in Psychiatry” chapter in the Encyclopedia Americana as well as Integrative Treatment for Borderline Personality Disorder: Effective, Symptom-Focused Techniques, Simplified for Private Practice. Dr. Preston is the recipient of the Mental Health Association’s President’s Award for contributions to the mental health community and the California Psychological Association’s “Distinguished Contributions to Psychology” award. He has lectured in the United States, Canada, Europe, Africa, and Russia.
Kenneth V. Hardy
Kenneth V. Hardy, PhD, is President of the Eikenberg Academy for Social Justice and Clinical and Organizational Consultant for the Eikenberg Institute for Relationships in NYC, as well as a former Professor of Family Therapy at both Syracuse University, NY, and Drexel University, PA. He’s also the author of Racial Trauma: Clinical Strategies and Techniques for Healing Invisible Wounds, and The Enduring, Invisible, and Ubiquitous Centrality of Whiteness, and editor of On Becoming a Racially Sensitive Therapist: Race and Clinical Practice.
Mary Jo Barrett
Mary Jo Barrett, MSW, is the founder and director of Contextual Change and coauthor of Treating Complex Trauma: A Relational Blueprint for Collaboration and Change and The Systemic Treatment of Incest.
John Gottman
John Gottman, Ph.D., was voted one of the Top 10 Most Influential Therapists of the past quarter century and was recently honored with the 2021 Lifetime Achievement Award by the Psychotherapy Networker. Professor Emeritus in Psychology at the University of Washington, Dr. Gottman is known for his work on marital stability and relationship analysis through scientific direct observations, self-report and physiology. He is the author or co-author of over 200 published academic articles and more than 45 books, including the bestselling The Seven Principles for Making Marriage Work; What Makes Love Last; The Relationship Cure; and Why Marriages Succeed or Fail. He is the co-founder of The Gottman Institute and Affective Software, Inc., which has created a tele-therapy technology that will live on cell phones, computers, and tablets to assist therapists in couples therapy and offer direct relationship building services directly to couples. Learn more at Gottman.com.
Salvador Minuchin
Salvador Minuchin, MD, is a contemporary psychiatrist who helped to develop family therapy and pioneered the field of structural family therapy (SFT).