Enjoy the audio preview version of this article—perfect for listening on the go.
Cure: A Journey into the Science of Mind Over Body
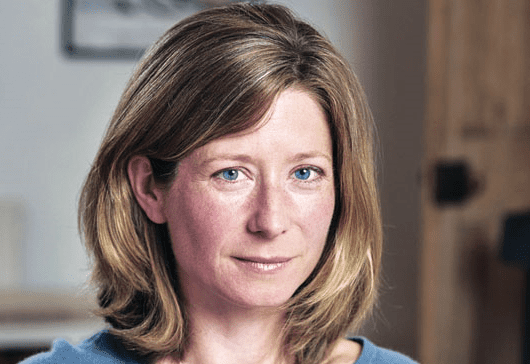
by Jo Marchant
Crown. 300 pages.
9780385348157
Science journalist Jo Marchant opens her new book, Cure: A Journey into the Science of Mind over Body, with a confession. Until she began investigating the intertwined ways mind and body can work together to enable healing, she’d dismissed most alternative medical treatments and mind-based therapies as unscientific nonsense. After all, for centuries, conventional medical wisdom had held tight to the assumption that mind and body were separate entities and never the twain would meet. Yet being scientific, Marchant realized, also means being open-minded to exploring and testing new hypotheses. She decided to find out what the evidence showed—and what it didn’t.
The result is a state-of-the art tour of mind–body medicine. Marchant’s research-based assessment appears at a tipping-point moment, when even the most mainstream medical institutions (Harvard, among others) and media stalwarts (think The New York Times) are increasingly studying, accepting of, and reporting on, the improvements in both mood and medical status that such treatments can bring.
That means that many psychotherapists are already familiar with some of the ground Marchant covers, especially practitioners who for some time have been successfully using mindfulness, meditation, and similar techniques for clients suffering from ailments ranging from post-traumatic stress disorder to anxiety, depression, and chronic pain. But Marchant brings readers up to date on the most recent studies and developments, especially in our understanding of the placebo effect, the well-known phenomenon by which people feel better after being given a fake treatment. She introduces us to the work of Italian neuroscientist Fabrizio Benedetti, who pioneered the study of how placebos can spur the body to action. The expectation that a pill will lessen pain can trigger the actual release of pain-killing endorphins, he found. Similarly, when he gave placebo medication to Parkinson’s patients, their brains became flooded with symptom-relieving dopamine. As Marchant writes, “Benedetti had chased a belief right down to an individual cell—demonstrating that in Parkinson’s patients, motor neurons fire more slowly after injection of a placebo, exactly as they do in response to a real drug.”
In another example, when visitors to Benedetti’s high-altitude lab in the Alps were given fake oxygen to help their altitude sickness, they felt better, and tests showed that they had experienced a real-time reduction in the high prostaglandin levels that cause such symptoms. All these responses were physiologically equivalent to those you’d expect if the patients had been given the real thing. But perhaps the interplay between the physical and the psychological shouldn’t be surprising. “Scientists are increasingly finding that psychiatric disorders such as schizophrenia or depression reflect structural abnormalities in the brain,” Marchant writes, “while neurological problems, such as Parkinson’s cause psychological symptoms as well as physical ones.”
What many readers may find even more surprising is the extent to which placebo effects can work even when the patient knows the treatment is phony. For a 2010 study, Ted Kaptchuk of Harvard enlisted 80 patients with long-term irritable bowel syndrome (IBS). Half of them received no treatment, while the other half were given capsules that they were told contained no active ingredient but that might work through mind–body, self-healing processes. The placebo-takers did significantly better. Kaptchuk had similar results in small studies of women with depression, and with migraine sufferers. He believes these effects result from the psychological meanings and interpretations we project onto particular types of treatments. Those meanings will differ according to our cultural beliefs about them, he says. For instance, while injections prove better placebos than pills in the United States, the opposite is true in Europe. In addition, in the burgeoning field of psychoimmunology, other researchers are experimenting with enlisting the principles of conditioning (as first shown by Pavlov) to train patients to respond to cues that can potentially help suppress overactive immune systems, which might otherwise reject organ transplants.
However, Marchant cautions that these findings don’t mean that everyone should throw their prescriptions away. Placebos have definite limits, she emphasizes. For the most part, they can do no more than help ease certain symptoms, such as pain, itching, diarrhea, and other discomforts. Bottom line: they won’t cure the underlying infection, disease, or condition causing those symptoms. And they don’t work all the time or for everyone. So given those limits, it’s hard to know what to make of the fact that you can buy placebo pills online.
Yet easing pain and discomfort is essential, and seems to be the hallmark of most of the mind–body medicine Marchant reviews. She interviews sufferers of severe IBS, who learned, under hypnotherapy, to influence the speed of their gut contractions, notably reducing their symptoms and allowing them to lead normal lives. She visits a hospital burn unit, where accident victims and combat veterans in excruciating pain gain respite by immersing themselves in virtual reality games. She quotes researchers who wonder if the burgeoning virtual reality market (represented most recently by Facebook’s purchase of Oculus) will lead doctors to incorporate it in pain management, perhaps allowing a decreased reliance on pain meds.
Certainly, amid today’s high levels of addiction to opioid pain meds, finding such alternatives is imperative, and mindfulness, meditation, and other stress-reduction techniques are becoming part of that new paradigm. In addition, research is ongoing to see if meditation—which has been shown to have the power to change the physical structure of the brain—may be utilized to slow the cognitive decline of old age and perhaps even ward off dementia. In yet another implication for public health and medical institutions as a whole, Marchant describes an increasing number of studies showing that more attention and TLC result in briefer hospital stays, better health outcomes, and lower bottom lines for patients and medical institutions alike. These are the most salient points in several chapters that may otherwise have the feel of being already overly reported on.
I’d say ditto for her section on the well-studied links between longevity and robustly active family and community ties if it weren’t for the fact that she juxtaposes these findings with their corollary: a perhaps equally strong association between being socially and economically marginalized and poor-health outcomes throughout the life span. To help both the elderly and the young, Experience Corps, a project overseen by the Johns Hopkins Bloomberg School of Public Health in Baltimore, asks isolated inner-city elders to volunteer as tutors for elementary school students in low-income neighborhoods. The personal bonds created between the generations has benefited all concerned. The students’ grades improved, and the elders found renewed purpose in their lives. Additionally, the seniors’ brain-imaging scans showed reversals in age-related brain damage. The hippocampus, which usually shrinks with age, grew larger.
Marchant’s concluding chapter focuses on how spirituality fits into the mind–body connection. Although she doesn’t believe in miracles, Marchant nonetheless goes to Lourdes, where she becomes one among many volunteers aiding ailing religious pilgrims who’ve come in search of a miraculous cure. What she witnesses instead is the miracle of social support, even from strangers, in easing stress and calming the mind of even the most distressed. Whether or not an individual finds solace in belief in God, we all benefit in mind and body from social connections that bind us together.
If there’s one common theme Marchant keeps returning to, it’s that “if we feel safe, cared for, and in control—in a critical moment during injury or disease, or generally throughout our lives—we do better. We feel less pain, less fatigue, less sickness. Our immune system works with us instead of against us. Our bodies ease off on emergency defenses and can focus on repair and growth.” She’s not a cheerleader for all forms of alternative medicine. She warns readers of the limitations inherent in even the most potentially potent mind–body possibilities, and she urges caution against fraudulent treatments that prey on patients’ desperation. But despite her initial skepticism, her book is filled with evidence that our minds and bodies both will thank us for harnessing their intertwined powers to help us heal.
Photo © Garry Simpson
Diane Cole
Diane Cole is the author of the memoir After Great Pain: A New Life Emerges and writes for The Wall Street Journal and many other publications.