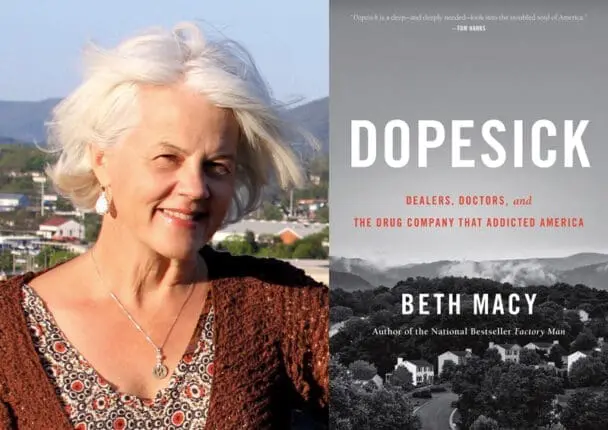
Dopesick: Dealers, Doctors, and the Drug Company that Addicted America
by Beth Macy
Little Brown
376 pages
978-0316551243.
In August 2016, author and journalist Beth Macy traveled to the Hazelton Federal Correctional Institution in West Virginia to interview convicted drug lord Ronnie Jones. He’d run one of the most extensive drug rings in the mid-Atlantic region, and his business had helped fuel the area’s spiraling overdose rate.
Macy, who lives in Roanoke, Virginia, a small-sized city adjacent to both the scenic Blue Ridge Mountains and the economically distressed former coal towns of Appalachia, was reporting on the devastation caused by the opioid epidemic, which had led to the deaths of more than 300,000 Americans over the previous 15 years. But beyond the astonishing numbers, she was carrying with her countless stories from grief-stricken mothers struggling with unanswered questions she was intent on posing to Jones. How could their children, some barely out of adolescence, have gotten so swept up with these drugs? How did their brains get so hijacked that they’d lie, cheat, and steal from their own families to score a fix? And why was effective treatment almost impossible to find, much less afford?
Perhaps predictably, none of that concerned Jones. From his point of view, jail time was just the price of business—and given the speed at which other dealers had already stepped in to replace him when he was arrested, that business wasn’t going away. Nor was he interested in the pain he’d caused the parents whose kids had died on the product he’d sold them.
That’s the heartbreak that beats through every page of Beth Macy’s Dopesick: Dealers, Doctors, and the Drug Company that Addicted America. A skillful and intrepid reporter, with a knack for getting people to open up to her, Macy traces the history of the epidemic, chronicles its devastation, and explores the barriers to treatment. As she tracks the ever-expanding wreckage across socioeconomic barriers, she emphasizes the human cost of the scourge.
With empathy and understanding, she focuses on the stories and struggles of several addicted teens and 20-somethings, along with their parents and extended families. She provides deft portraits of medical and mental health providers stretched to their limits by overwhelming patient loads and meager budgets. And she portrays the bewilderment of suburban communities caught between denying the problem in their midst and not knowing how to cope with or limit the damage.
Dopesick, Macy explains, is slang for the excruciating symptoms of sweats, chills, vomiting, and diarrhea brought on by drug withdrawal—a state so unbearably fraught with pain and anxiety, her interviewees attest, that addicts craving their next fix will do almost anything to avoid it. Yet the equally troubling sickness she diagnoses is the blindness of government and public health officials to the early stages of the epidemic, when they could’ve limited the harm to come.
Macy dates the start to 1996, with the introduction of OxyContin, which was aggressively marketed by Purdue Pharma, its producer, as a potent pain reliever that would last 12 hours—at least twice the duration of any other available pain medication. Further, while touting the idea that pain was being undertreated in the medical community, the company insisted that the drug would be resistant to abuse on the streets because it didn’t provide the immediate euphoric rush of a short-acting narcotic. OxyContin was the ideal product to bring needed relief, sales reps promised doctors, as they wined, dined, and treated them to other freebies.
No matter that these medical claims were backed by scant research, if any. Amid Purdue’s big budget advertising and promotional blitz, questions about promises that sounded too good to be true went mostly unheard and unanswered. Sales boomed, bringing soaring bonuses to successful sales reps and outsized profits to the company’s bottom line. By 2001, OxyContin had become the country’s most frequently prescribed brand-name opioid pain pill—and though Purdue and health officials weren’t yet owning up to it, among the most abused.
Rural Appalachia, with its closed factories and mines, was one of the first and hardest-hit areas. The jobs were gone, but the injuries and disabilities suffered by the workers remained.
Believing the hype that OxyContin was risk free, physicians started routinely prescribing lengthy, refillable doses. What harm could it do?
Plenty. It became an open secret that OxyContin pills could easily be crushed and then injected or snorted, yielding an immediate and powerful high. It also turned out that for a great many patients, the drug’s promised 12-hour effect didn’t pan out, leaving them to suffer simultaneously from their physical pain and the start of withdrawal symptoms, a double whammy of sickness that left them begging for the next fix, and then the next. Unemployed, needing money, and now dope, too, patients started becoming hustlers, selling and bartering their own pills and prescriptions, and running scams and schemes to support their habits, even if it meant bankrupting their families.
These early casualties in so-called flyover country remained mostly invisible to the rest of the nation. And even where it was happening, the problem remained underground, not just because of the shame and stigma of addiction, but because small-town media outlets that might’ve covered the story and sounded alarms were being shuttered as their traditional platforms were being upended by the digital boom and subsequent budget cuts.
Finally, when local doctors and health officials did speak up, Purdue felt no pressure to respond, given that no one seemed to be listening. In retrospect, its consistent denials of wrongdoing echoed those of tobacco companies that were once effective in disavowing the negative health consequences of smoking. When, in 2007, federal prosecutors did succeed in forcing Purdue to admit to its fraudulent marketing and pay $600 million in fines, the demand for opioids had already spread so far that cutting it off created an even worse backlash: drug dealers switched from selling OxyContin to selling heroin.
And so the juggernaut of the epidemic continued. Macy best captures the human cost of addiction in a quote from a farmer who’d lost his land to his habit: “Nothing’s more powerful than the morphine molecule, and once it has hooks in you, nothing matters more. Not love. Not family. Not sex. Not shelter. The only relationship that matters is between you and the drug.”
The cruel dynamics of that relationship are on display throughout the book, with Macy portraying distraught parents’ struggles to get their children to break up with their addictions, with mixed results. Many of these parents had felt protected in their suburban, upscale neighborhoods from the drug problems that they’d persuaded themselves only happened elsewhere.
Among the first to be dissuaded of this myth was Robin Roth, a registered nurse whose son Scott had died from a heroin overdose in 2010 at the age of 21. “You think of heroin as seedy street slums, but that’s not at all how it started,” she told Macy. Someone had handed him a joint laced with heroin at a high school party when he was 16; by the time he was 17, he was shooting up and hooked. She put him in rehab, took away his car, and removed all the doors in their house so he wouldn’t be able to shoot up secretly, but nothing worked.
He received the fatal heroin dose from an old drug buddy from school, Spencer Mumpower, who’d himself failed to kick his drug habit after no less than 15 failed attempts at rehab. In prison for his role in Scott’s death, he finally succeeded in getting clean, and his mother, a jewelry store owner, decided to eschew shame and secrecy to become an informal counselor to distraught parents seeking a sympathetic ear.
One such parent was Drenna Banks, who ran a successful insurance business with her husband. She once judged family friends whose son had overdosed on heroin, thinking, Why can’t you control your kid? Then her 19-year old son Colton died of a drug overdose while she and her husband were attending church. “At first, you’re just so embarrassed,” she confessed to Macy. “You think you’re doing right as a parent, but then these drugs take over their life, and nobody talks about it because it’s this dark, hidden secret.” Her friend Jamie Waldrop, a Roanoke civic leader and wife of a prominent surgeon, saw two sons through repeated stints at rehab. “Until they go off to rehab, you don’t realize just how dysfunctional your life has become,” she said. The family spent $300,000 on rehab alone.
From these stories, Macy distills a variety of practical prevention tips for families with anyone at risk. “Rid your medicine cabinets of anything that has codone, indicative of morphine components, in the name,” she writes. “Set rules and hold kids accountable when they break them, even if it means they go to jail”—a tough-love strategy that ultimately worked for Spencer Mumpower, but may not for everyone. She also warns of the possible dangers of freely prescribing medications for ADHD. “Almost to a person, the addicted 20-somethings I met had taken attention-deficit medication as children, prescribed pills that as they entered adolescence morphed from study aid to party aid”—an aide that could be traded for money or harder drugs.
But the most apparent need that emerges in the book is for effective, affordable addiction treatment, and for rethinking the unending obstacles blocking placement. Those hurdles include an insufficient number of treatment facilities, high costs and limited insurance coverage, a dearth of counselors and physicians specializing in addiction medicine, and an ideological divide among treatment providers themselves over what works best—12-step type abstinence programs or Medication Assessment Treatment (MAT), in which the patient is given medication in combination with counseling and therapy.
Current research shows that MAT combined with psychosocial support is most effective. As for which medication, methadone was the first substance used to quell opioid cravings; now, Suboxone is favored as safer. Regardless of which protocol is used, however, access to affordable treatment facilities remains a problem. Tragically, more than one of the young addicts whose stories Macy recounts dies just as a coveted place in a rehab facility comes open. Since most of these drug victims had been in and out of different types of treatment before, it’s unclear whether this time would’ve worked. What is clear is that even though at times it’s difficult to keep track of the many overlapping stories told by Macy’s interviewees, it’s impossible not to be affected by this book.
Diane Cole
Diane Cole is the author of the memoir After Great Pain: A New Life Emerges and writes for The Wall Street Journal and many other publications.