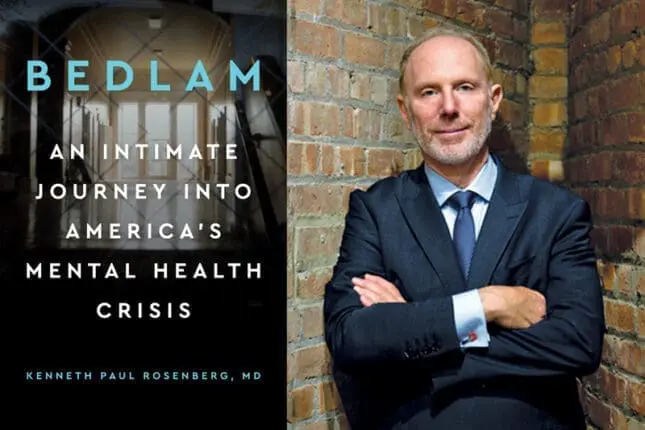
Bedlam: An Intimate Journey into America’s Mental Health Crisis
by Kenneth Paul Rosenberg
Avery
240 pages
“My family’s tragedy is an American tragedy. My family’s shame is America’s great secret.” That is how the psychiatrist, author, and documentary filmmaker Kenneth Paul Rosenberg begins his disturbing and deeply personal investigation into why our country seems unable to care for, and too often even care about, the estimated 11.2 million people age 18 or older who suffer from serious, debilitating mental illness. Bedlam: An Intimate Journey into America’s Mental Health Crisis is the title shared by his recently published book and his documentary, which received its premiere at the Sundance Film Festival earlier this year and is slated for broadcast on PBS in April. They both demand our attention.
A member of Rosenberg’s own family of origin was among the 20 percent of Americans who, according to the National Institute of Mental Health, experience mental illness. Growing up in Philadelphia, he watched his older sister, Merle, transform from a charmingly outgoing if also irascible adolescent into an increasingly erratic woman suffering from ever more frequent psychotic episodes, which included paranoid and hallucinatory rages.
Hospitalizations, psychotherapy, medications, shock therapy—even when these treatments helped, she refused to stay with them, sometimes because of the drugs’ side effects and other times because she rejected the very idea that she needed help. Periodically, she’d disappear from home, which is how it happened that one day, as he drove through Rittenhouse Square, Rosenberg realized that the homeless woman on the sidewalk was his sister. Still, he kept her illness a secret from others, their family front of denial attesting to the shame and stigma that serious mental illness carries.
But in the years since his sister’s death, at the age of 55, in 2006, Rosenberg has devoted himself to documenting and exposing the catastrophic inadequacies of our mental healthcare system. He views this ongoing lapse of communal compassion and governmental responsibility as “the greatest social crisis of our time.”
Most people tend to ignore the increasing numbers of mentally ill people who live, mostly untreated, on our streets; Rosenberg’s achievement is that he makes us see them, using Los Angeles as a microcosm of what’s happening across our country. He estimates that 15,000 people experiencing homelessness on the LA city streets are struggling with serious mental illness, and the Los Angeles County Jail doubles, he says, as “the largest mental treatment facility in the nation.” Many have landed there after police officers have responded to reports of some manifestation of their illness in the form of out-of-control behavior, from breaking a window to jumping out one, verbally hassling passersby to physically assaulting someone. But the offense itself can matter less than the consequence: an arrest record usually means more jail time and higher bail, which people without a job or a home have no way to pay. As one research psychiatrist told Rosenberg, “The mentally ill end up in jail because they get arrested, mainly for petty crimes, and as a result they cycle in and out of the jails without ever getting any sustained and consistent treatment.”
Given that most officers aren’t trained to deal with psychiatric illness, confrontations often lead to injury or fatality. “Roughly a quarter of the people shot by police have a history of mental illness and a vastly disproportionate number of them are African Africans,” Rosenberg reports. Police intervention often ends in officers physically restraining or handcuffing those in the throes of delusions as they haul them away. Such incidents often act as further traumas, setting the scene for an even more fearful or contentious interaction the next time the police land on the scene.
Rosenberg details the stories of a representative handful of the many people who toggle in this way between living on the streets and serving time in jail. In one chapter, we meet 20-something Johanna in the psychiatric emergency room, where the police have brought her in the throes of her latest bipolar mania. This is one of the 10 hospitalizations she’s undergone that year, even as she struggles to stay on her meds, live independently, and make sense of her situation. She tells Rosenberg, “I’m college educated. I don’t have any [physical] disabilities. I don’t have racism going against me. I don’t have a violent background. I didn’t grow up with parents who beat me or anything. . . . If I can’t make it, what about everyone else?”
Indeed, each of Rosenberg’s case histories dramatizes how, across age, social class, racial background, or education level, it’s all too often difficult for victims of severe mental illness to receive the sustained help they need. Todd, 55, struggles with bipolar disorder. He’s black, HIV-positive, and living on skid row between years-long stints in jail. “I don’t want to die on the streets,” he tells Rosenberg. So he’s overjoyed when, after months of working with a nonprofit organization that finds affordable housing for the homeless, he finds a place of his own. But soon after, another arrest on a petty drug offense lands him back in jail. Though he’s facing kidney and liver cancer, as well as a declining T-cell count, the judge refuses to waive bail on compassionate grounds. Unable to pay both bail and rent, Todd loses the apartment and ends up back on the street.
Rosenberg intersperses these and other case histories with the story of how our national approach to mental health problems became an American version of Bedlam, the notorious British psychiatric hospital that became a synonym for chaos and horror. According to Rosenberg, the responsibility for this contemporary Bedlam is shared by a large cast of characters. Some were well-meaning, like the politicians and policymakers in the 1950s and 1960s who rightly condemned the run-down warehouse-like conditions of state mental health institutions and shut them down. But once those primarily inpatient institutions were gone, the proposed government funding to replace them with predominantly outpatient community mental healthcare centers never materialized.
As a result, the few clinics available were unable to serve enough patients. And because their treatment model was based on the overly optimistic but ultimately misguided belief that inpatient psychiatric stays would no longer be needed (psychotherapy and medications being sufficient), hospital beds for those suffering from serious mental illness became either unattainable or unaffordable. Rosenberg also blames Big Pharma for pulling back on neuropsychiatric drug development, which has limited the introduction of new medications—a culpability for which he should also fault our government for its aggressive, decades-long budget cuts of medical research into psychiatric disease. And thus we arrive at the current debacle, in which our jails have become de facto mental health institutions, housing approximately 383,000 individuals with severe psychiatric disease.
Rosenberg calls this the criminalization of the mentally ill, recreating “the dysfunctional, abusive dynamic that once plagued the institutions deemed so inhumane that they needed to be shut down in the 1960s.” At the LA County Jail, he estimates that about 25 percent of the men and 40 percent of the women require mental health treatment, which, if it’s given at all, is described to him as “beyond inadequate.”
Rosenberg does find some glimmers of hope. One is assisted outpatient treatment (AOT). Modeled after drug courts, which send drug abusers not to prison but to mandatory substance programs, AOT makes possible what one of its adherers, Texas probate judge Oscar Kazen, calls “therapeutic jurisprudence.” It allows judges to sentence people suffering from severe mental illness to mandatory, court-monitored treatment for up to a year. Limited to those who have shown an inability to remain on treatment through a history of multiple arrests, incarcerations, and hospitalizations, it’s now a legal alternative in most states.
Critics question the ethics of making such treatment compulsory. As Rosenberg writes, “That a judge can dictate the terms of long-term medical care that can possibly involve involuntary institutionalization and the administration of mind-altering medicines with serious side effects is concerning, right?” But Rosenberg has seen such programs work. Thanks to this alternative, Monte, whose schizophrenia over the decades has sent him shuttling back and forth from jail to the care of his sister and their extended family, is now staying on his meds and going for regular talk therapy appointments. He’s even holding down a seasonal job selling Christmas trees.
AOT has won endorsements from numerous groups, including the National Alliance on Mental Illness and the International Association of Chiefs of Police. Research has also shown a number of benefits: participants’ greater adherence to taking their meds; reduced arrests, hospitalization, and homelessness rates, resulting in lower costs to the public; fewer violent crimes committed by the severely mentally ill, leading to a higher level of public safety; and participant self-reports of better functioning and the ability to stay on their meds.
Another promising idea is for families to draft a psychiatric advance directive that details what treatment a person with mental illness consents to, should that person not be in a state to express those wishes. Rosenberg hails this idea as “an opportunity to write up what approaches have and have not worked in the past so that providers have a more complete history to inform care decisions.”
Throughout, Rosenberg emphasizes the importance of early diagnosis and a quick start to appropriate treatment. The reason: the longer a psychiatric illness progresses without treatment, the more intractable and severe it becomes over time. “It’s no exaggeration to say that untreated psychosis is actually toxic to the brain (neurotoxicity),” Rosenberg writes, “as overactive brain systems destroy cerebral matter, with excess dopamine, catecholamine, and stress hormones seen as potential bad actors.”
One solution is greater awareness of the symptoms of psychiatric disease and the pathways for treatment that are available. To that end, Rosenberg devotes the book’s final chapter to practical advice for patients and their families. It’s one among many reasons to recommend this book to anyone needing guidance on these issues. Writing this book made him an activist, he says. Read it, and you may become one, too.
Diane Cole
Diane Cole is the author of the memoir After Great Pain: A New Life Emerges and writes for The Wall Street Journal and many other publications.