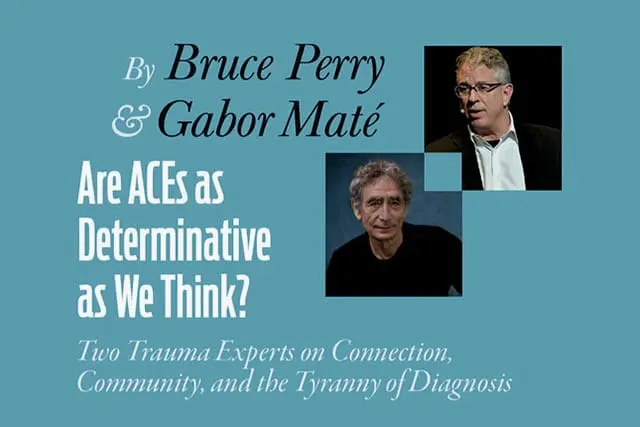
Last year, as part of a special free training on healing the wounds of trauma, Psychotherapy Networker hosted a discussion between two lions of the field. Bruce Perry is regularly cited as the world’s leading expert on early trauma. He spoke with influential trauma expert Gabor Maté. The following is excerpted from their talk.

Gabor Maté: American psychiatrist Thomas Hora once said, “Once you know the how, then you get the what.” In other words, once we have a framework for understanding something, the techniques follow. Techniques are secondary to understanding. And nobody has been more instrumental in my understanding of mental health, child development, and brain development than Bruce Perry.
What I greatly admire about you, Bruce, is that you’re not afraid to challenge the dominant perspective. You say that adverse childhood experiences (ACEs) are of consequence, but not as determinative as most people think. Where did you get that idea?
Bruce Perry: My working group now has data on the developmental history of connectedness and adversity in 100,000 individuals. When we look at their current functioning, we find the best predictor of how well they’re doing is how well they’re connected right now. You can have a horrific history, but if in the present moment you’ve got good relationships, are connected to your culture, and feel like you belong to a community, you have a tremendous therapeutic buffering. With that buffering, healing opportunities take place.
Similarly, with people who are struggling, how connected they were to family, community, and culture on their pathway to the present is a better predictor of their struggles than their ACE score. If you had some of those connections, while you might have absorbed some toxicity in your early life, you also had tremendous opportunities to counteract the effects.
Unfortunately, our current medical economic model for mental health is fundamentally disruptive to the capacity to create an enduring connection because we view therapists as interchangeable. You see therapist one and suddenly oh, you’re going to go see therapist two, then therapist three. And they may all be great clinicians, but every time you start working with someone new, you’re disrupting the mutative element of therapy, which is the relationship.
Underlying this is the reality that this model doesn’t support therapists in the ways they need to be supported to do the enduring relational work that leads to the most positive change. That’s the moral injury that we put many therapists in by having them try to make a living in the current medical economic model. You see this especially if you work in a clinic and have a requisite number of clients you need to see, and a requisite amount of time you’re supposed to see them, and you get third parties saying, “You’ve seen them 20 times. Why haven’t you cured them?”
I think it’s tough to be a therapist in this current climate.
Maté: I think mental health professionals often work under the tyranny of diagnosis and the primacy of the DSM. Diagnoses may be helpful as descriptors, but they’re never explanations. We assume that the diagnosis explains something, but at best it just describes how it manifests.
You told me that you were asked to contribute to one of the editions of the DSM, and you said no. You also said that you haven’t used diagnoses in your work for a long time, and it’s much more effective that way.
Perry: When we put people in buckets based on their symptoms, we ignore equifinality and multifunctionality, two important principles in development. Basically, these say that there are multiple physiological pathways to the same symptoms. You can have an attentional problem because of lots of different physiological problems, and you can also have one problem in a physiological system that leads to multiple symptoms. The combination of those two realities lead to complete chaos when it comes to trying to understand what’s really underneath a current DSM label.
We really have to abandon this way of thinking about studying and treating people based on diagnosis. Every single clinician knows exactly what I’m talking about: if they really guided their treatment approach based on diagnosis, they’d be very frustrated.
Maté: A lot of psychologists working in schools are having to come up with a diagnosis in order to justify getting help for a child.
Perry: This is where the systems have created a toxic reality. A bright, well-intended, well-trained, and otherwise effective clinician working in a school realizes that the only way Billy is going to get extra help is if he gets a certain label, even though that label doesn’t mean crap. The same thing happens with clinicians doing clinical work they can’t get paid for unless they affix a certain label to a client. It’s created an unhealthy alliance between the economic model and practice.
Maté: Along those lines, neurodiverse has become a popular label these days. What effect do you think the neurodiversity movement is having?
Perry: I think it’s moving us in a good direction because it’s helping people see that you can exist in this world in different ways and have different sets of gifts—and that the problem isn’t with the person, it’s with the way society or its systems view that person.
As you often point out, Gabor, we’re all different. We all have unique wounds, quirks, worldviews, and distortions. Rather than everybody feeling like they’re inadequate and abnormal, we need to recognize that that’s the way human beings are.
Maté: Your books—including your most recent one with Oprah, What Happened to You—have helped increase the public’s trauma awareness. But there is still a lot of resistance, even in our own field, to the idea that trauma can play such a big role in our development. Do you think we’re actually moving forward in this respect?
Perry: I’m optimistic that we are. Systems are kind of biological organisms. They have their own rules of how they work, and they’re very resistant to change, just like we are. But I do feel like we’ve helped push things in the right direction.
Gabor Maté
Gabor Maté, MD, a family practitioner for over three decades, is the author of four bestselling books, including When the Body Says No: Exploring the Stress-Disease Connection and In the Realm of Hungry Ghosts: Close Encounters with Addiction. His upcoming books include The Myth of Normal: Illness and Health in an Insane Culture.
Bruce Perry
Bruce Perry, MD, PhD, is the author, with Maia Szalavitz, of The Boy Who Was Raised as a Dog, based on his work with maltreated children, and Born For Love: Why Empathy Is Essential and Endangered. His most recent book, What Happened to You? Conversations on Trauma, Resilience, and Healing, was coauthored with Oprah Winfrey. Formerly, he was faculty at the University of Chicago and Baylor College, and chief of psychiatry at Texas Children’s Hospital. Currently, he’s the principal of the Neurosequential Network and an adjunct professor in the Departments of Psychiatry and Behavioral Sciences at the Feinberg School of Medicine at Northwestern University.