Editor's Note
Livia KentFacing the Past as a Parent
How Our Worst Moments Can Stop Intergenerational TraumaFor one trauma therapist, parenting turned out to be the ultimate trial by fire—and a path to healing and wholeness. Read more
The Dangers of a Phone-Based Childhood
Are We Protecting Kids in the Wrong Way?What happens when a whole generation of children are overprotected on the playground and underprotected online? Read more
“Gentle Parenting” a Fierce & Feisty Kid
When One-Size-Fits-All Scripts Don’t WorkThe prescriptive, one-size-fits-all version of “gentle parenting” promoted on social media may work with many kids, but for parents of “big reactors,”... Read more
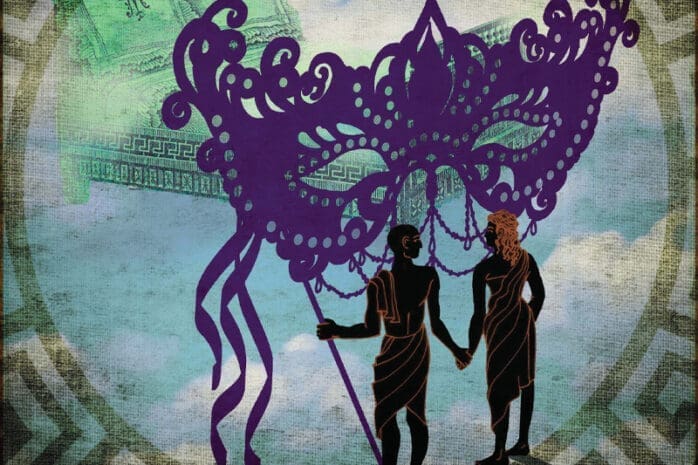
“She Looks Just Like You”
What Are We Not Seeing with Donor-Assisted IVF?Understanding the impact of “resemblance talk” and the challenge of “parental claiming” can help the parents of donor-conceived children feel... Read more
The Surrogacy Partnership
Navigating a Complicated, Intimate ArrangementBuilding a trusting relationship with a surrogate requires a wide array of interpersonal and self-regulation skills— and can be the ultimate exercise in... Read more
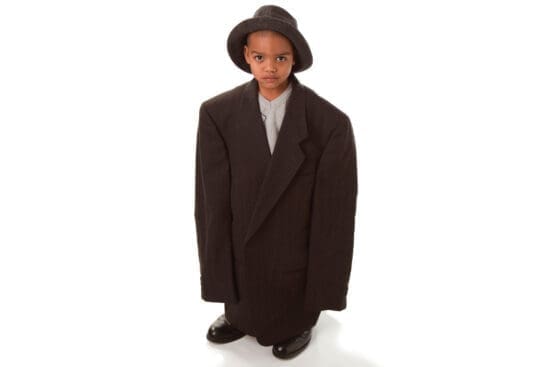
The Parentification Trap
Growing Up Too Fast as a Child of ImmigrantsHow does it impact the development of second-generation kids when their sense of self is inextricably tied to meeting the needs of parents and elders? Read more
Countering the Mommy Brain Stigma
The Benefits of Maternal Neuroplasticity at WorkRather than a deficiency, “mommy brain” is an asset—and therapists can help their clients embrace it in the workplace. Read more
Extra Feature
An Autobiography of Trauma
The Developer of Somatic Experiencing Releases His Own “Body Memory”When the world-renowned developer of Somatic Experiencing begins feeling persistent disturbing sensations come up from childhood, he realizes it’s time to... Read more
Sue Johnson changed the field, creating a ripple effect of healing that continues to transform countless relationships. In a mosaic of anecdotes drawn from the... Read more
Departments
The Cultural Competence Dilemma
How Much Can We Rely On a Shared Identity with Clients?Demystifying Walk and Talk Therapy
How to Get Outside With ClientsSexual Fantasies in Couples Therapy
The Art of Encouraging Erotic ImaginationVienna Pharaon on Family-of-Origin Work
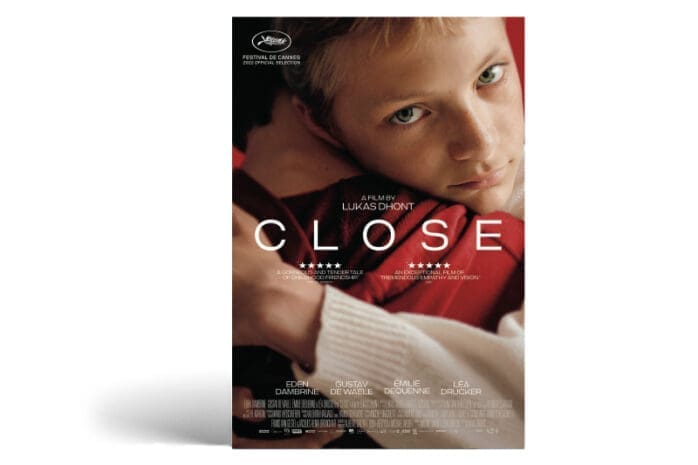
The Importance of Looking back to Move ForwardBoys Holding Hands
How Are We Policing the Beauty of Male Intimacy?An Apple Seed and Trained Monkeys
Growing Up Under the Influence of My Big Sister's ImaginationPractice Tools: July/August 2024
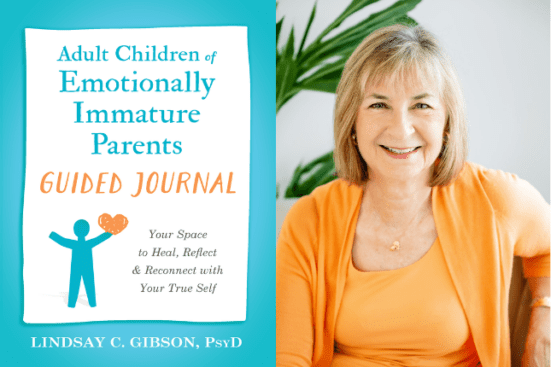
The best from across the field of psychotherapy . . . on us!This month’s selection is from Lindsay Gibson’s Adult Children of Emotionally Immature Parents Guided Journal: Your Space to Heal, Reflect and Reconnect... Read more