She wasn’t responsive to my voice or my soft touch. Her face was pale, her body was limp, her breathing was rhythmic and shallow. Should I call the medics, I wondered, or have her mother carry her out of my office? Luckily, she was my last client for the day, so I had time to figure out what to do with this unresponsive teen. I was seeing dissociation in its extreme form: the body shutting down in a “freeze” position, the way some wild prey respond when threatened by a predator. But what in our session had 17-year-old Trina perceived as “predatory”?
Though there had been a casual conversation about college plans and a boyfriend, there had been no talk of her early sexual abuse memories with a grandfather with whom she no longer had contact. After three years of treating her for dissociative behaviors, including sudden regressions, amnesia, and dazed states, I thought we’d moved beyond such an extreme response to stress on her part.
Trina was demonstrating a “dissociative shutdown,” a symptom often found in children faced with a repeated, frightening event, such as being raped by a caregiver, for which there’s no escape. Over time, this response may generalize to associated thoughts or emotions that can trigger the reaction. Although the child’s body may be immobilized, her mind remains active and can invent solutions, often retreating into an imaginary world, where bad things aren’t happening. With time and practice, the mere thought of needing to escape a situation may trigger a self-induced hypnotic retreat, along with a primitive freeze response.
According to Bruce Perry, senior fellow of the ChildTrauma Academy in Houston, these kinds of episodes are best understood as a dysregulation of the central nervous system’s opioid systems, which have been repeatedly activated by extreme stress. This response then becomes an enduring “trait,” so that small reminders of trauma can stimulate these dramatic alterations in consciousness. Perry points out that medical professionals often are puzzled by this kind of shutdown and may diagnose it as “syncope of unknown origin,” “conversion reactions,” or “catatonia.”
Working with dissociative children and teens can be unnerving for therapists, particularly in view of such extreme symptoms. A basic theoretical understanding of dissociation can demystify even this kind of sudden in-session event. But as important as it is to have a theoretical understanding of what’s happening, a clinician needs a pragmatic, strength-based, problem-solving focus to feel prepared to treat such entrenched dissociative reactions in children and teens.
Most children experiencing dissociation don’t have as little control as Trina did at this juncture. Usually, signs of dissociation can be as subtle as unexpected lapses in attention, momentary avoidance of eye contact with no memory, staring into space for several moments while appearing to be in a daze, or repeated episodes of short-lived spells of apparent fainting. As they move along an intensity spectrum, some young clients may have alterations in identity, with sudden regressions or rage-filled episodes, and little awareness of their behavior.
There’s still little consensus about how dissociation develops in traumatized children, but it’s been linked to disorganized attachment, often characterized by blank looks, avoidant eye gaze, and shifting affect. Frank Putnam, director of the Mayerson Center for Safe and Healthy Children at Cincinnati Children’s Hospital, has theorized that, while most infants learn to shift flexibly between emotional states over time, trauma-based states are marked by inflexibility and impermeability. According to psychologist Silvan Tomkins, children learn to rely on “affect scripts,” sequences of automatic behaviors that help them avoid experiencing such painful affects as fear, shame, or disgust—the kind of deeply disturbing feelings aroused during sexual abuse or other traumatic experiences with caregivers. The traumatized child learns to avoid overwhelming emotional pain through dissociation. As a consequence, these children can fail to develop the basic building blocks of identity and consciousness.
The reversal of dissociative states requires a therapeutic relationship in which the child can feel safe and clearly distinguish between the present environment and the traumatic past, while developing the deep, embodied conviction that the future doesn’t have to mirror what he or she has already been through. From years of experience working with children like Trina, I knew that my job was to help her discover alternatives to her avoidance response, understand and learn to tolerate its triggers, and find ways to override the automatic physiological escape tendency over time.
Handling the Emergency
When I asked Trina’s mother to come into my office, she first gently shook her daughter, saying “Trina, session is over” in a singsongy, motherly tone. No response. In a quiet, hypnotic tone, I suggested to Trina that she’d find herself growing more and more awake, ready to face hard roadblocks in her life. No response. Then Trina’s mother and I decided to call 911. Her mother, apparently accustomed to this strange behavior, was surprisingly calm. When the medics took Trina to an emergency room, I expected that she’d wake up as they transferred her to the stretcher and then the ambulance, but she didn’t.
Two hours later, my cell phone rang. It was Trina. “Dr. Soybean (her playful name for me),” she implored, “Please tell the hospital doctor that I don’t need psychiatric admission, and that I’m not crazy!” As relieved as I was to learn that she’d awakened from her dissociative slumber, I saw a great opportunity to move her forward therapeutically. Whenever my child clients ask me for something, I find a way to ask them to do something in return that will be a therapeutic advance for them. So I asked Trina to come to my office first thing in the morning, and explained that if she could successfully describe what happened right before her dissociative shutdown, she could avoid the hospitalization. If, however, she was unable to uncover the feelings that led to this self-defensive reaction, it would make sense for her to go the hospital after the session. Trina agreed to this.
The next session centered on the kind of “fishing expedition” often required with dissociative patients. Blocked from the feelings that usually help people string together a coherent narrative explaining their experiences, dissociative clients’ responses often appear as mysterious to them as they do to others. Trina remembered that we’d talked about her high-school science project, her ambition to be a biochemist, and a boyfriend she was outgrowing. I suggested that something else in our conversation had awakened her old feelings of being helpless, frozen, and unable to move forward. She acknowledged that was true but remained mystified about what had triggered the old sense of being trapped.
I asked her to focus on that feeling of being trapped and as Trina got in touch with it, she became agitated and nearly mute. As she struggled, I modeled slow, rhythmic breathing and softly said, “Breathe with me. We’ll get through this together.” She took my cue and followed my slow breathing. “Where are you feeling this in your body I asked?”
“In my chest—it’s tight,” she said.
I used a familiar image to help her counter the sense of constriction in her chest. “Let’s imagine together that you’re out in the woods near your house and breathing the fresh fall air,” I said. We stayed with this image for about five minutes, and then I redirected her.
“Whatever’s happened, we can work together so you can handle it. We can find a solution, no matter how scary the trap feels.” I’ve learned that blocked memory usually returns when the therapist provides safety and confident reassurance that the information is tolerable, so I asked, “If you had to guess who it was about, would you guess your mother, your boyfriend, or your father?” Sometimes “guesses” allow the unconscious mind to express itself.
“I don’t really know,” she said, “but if I had to guess, it would be about my father,” she said.
“Something he did or something he said?” I wondered with her.
“I don’t know,” she said, “but he always says stupid things to me, so he probably did say something.”
“Think about your father saying stupid things, and tell me what you feel,” I said.
“My chest feels tight” she said, “and I feel trapped.”
“You aren’t trapped,” I reassured her. “Your whole life is ahead of you. Every day you’re more and more free. Soon you’ll be 18, and have the freedoms of an adult.” My comment about her future, which she faced with both anticipation and anxiety, was right on target.
“That’s it!” she said, “I remember.”
Trina’s parents were divorced, with joint custody. With a shaking voice, she told me that her father had threatened to withdraw college funding if she didn’t agree to overnight visits at his house, where her early abuse had occurred. She’d visited him willingly over the years when he put no real pressure on her, but the controlling nature of his new demand aroused the hopeless feeling she’d experienced when her grandfather’s abuse had seemed so inescapable. The overwhelming fear she’d experienced the day before seemed to encapsulate a central dilemma faced by all child survivors, now heightened by her approaching transition to adulthood: could she grow up, go to college, and be normal? or was she stuck forever in the traumatic past? It was crucial to find a way to support her belief that she could move on in life and escape the traps of her past.
Now that Trina had explained her dilemma, we began to brainstorm practical solutions, discussing ways she could stand up to her father. Ultimately, she decided she’d like me to serve as an intermediary to help him understand why presenting his demand in this authoritarian way triggered her old symptoms. In a subsequent session, I told him how she experienced his attempt to influence her through his control of her college money. He insisted he hadn’t really intended to withhold the funds, he was only emphasizing to her that he “could.” In a subsequent family session, with my prompting and direction, he promised her he’d pay for college, and that he’d never use this threat again. For her part, Trina promised him she’d visit him as her schedule allowed. She never experienced that degree of dissociative shutdown again.
Follow-Up
Over time, Trina learned to believe that the brighter future she dared imagine for herself was possible. Her treatment revolved around learning to combat her automatic tendency to dissociative avoidance and repeated recommitment to her belief in a positive future, whatever challenges she faced in her life. Through her college and postgraduate education, she succeeded, using her skills in affect tolerance, identifying emotional triggers, and self-awareness to navigate dismissive teachers, rude boyfriends, and even the tragic death of a close friend. She stayed in my practice for six years, maturing from a frightened, avoidant girl who had trouble attending school to an aware, insightful survivor.
Today, Trina is an accomplished medical professional, married, with a young child of her own. When asked about her recollections of her early treatment, she says, “Yes, I was a weird kid, but you knew what to do about it.” She quickly changes the subject, but proudly shows me pictures of her new son, who she assures me is developing beautifully, “without dissociation or other wacky stuff.”
Case Commentary
By David Crenshaw
Working with extreme forms of dissociation is a demanding and often anxiety-provoking therapeutic challenge. In the face of extreme symptoms that can seem quite bizarre, the therapist must have the experience, skill, and emotional steadiness to communicate both a clear sense of direction and a conviction about what needs to be done. In the morning-after crisis interview with Trina, Joyanna Silberg displays all those qualities as she creates the kind of emotional bond and sense of safety that enables Trina to return to adequate coping. I question, however, whether the same qualities might have been more patiently employed the night before to help Trina avoid her trip to the emergency room.
In crisis moments, seemingly small shifts in language and affect can have major impact. I was struck by the difference in Silberg’s intervention the night of Trina’s dissociative shutdown and her more effective response in the next day’s follow-up session. In the first instance, Silberg describes her response in this way: “In a quiet, hypnotic tone, I suggested to Trina that she’d find herself growing more and more awake, ready to face hard roadblocks in her life.” The following day, Silberg is far more concrete and makes better use of her strong therapeutic alliance with Trina, as clearly conveyed in her instruction, “Breathe with me. We’ll get through this together.” I can’t help but wonder if the ER trip the previous night could have been avoided if Trina had heard something as powerfully reassuring as, “Breathe with me” and “We’ll get through this together.”
In the session the following morning, Silberg, with conviction and evident affect, simply and unequivocally says to Trina, “You aren’t trapped.” It’s then that Trina is empowered to remember the conversation with her father that had triggered her dramatic shutdown. Silberg reinforces her forceful statement with some powerful suggestions, including: “Your whole life is ahead of you. Every day you’re more and more free. Soon you’ll be 18, and have the freedoms of an adult.”
I was puzzled by Silberg’s response to Trina’s call from the ER. She describes Trina’s request to help her avoid hospitalization as an example of a “client ask[ing] me for something.” Silberg explains that in such situations she “find[s] a way to ask [child clients] to do something in return that will be a therapeutic advance for them.” This leads her to ask Trina to come for a session the following morning and identify the exact moment that triggered her “dissociative shutdown.” I didn’t understand the rationale that identifying the exact trigger moment would determine whether or not psychiatric hospitalization was needed. If the therapist is asking the client to come to her office the next day to pinpoint the exact moment of being triggered, surely she believes her patient is capable of outpatient therapy. If the client was unable to identify the exact trigger moment in that session, would that really be an adequate justification of psychiatric hospitalization?
Fortunately, the follow-up session is quite productive, reflecting the skills and strengths of both therapist and client. Ultimately, I think the validation of Silberg’s work with Trina and the quality that’s needed to help clients experiencing extreme symptoms like hers is embedded in the adult Trina’s retrospective comment on what her therapy experience meant to her: “Yes, I was a weird kid, but you knew what to do about it.” Clearly Silberg created the sense of safety, trust, and optimism that made it possible for Trina to move on with her life, despite her early abuse.
Author’s Response
I appreciate David Crenshaw’s thoughtful comments. Perhaps I described too quickly the efforts her mother and I made to awaken her the evening before. It was about 45 minutes of intense intervention before her mother and I made the decision to call the medics.
In most outpatient offices, I’d guess, therapists wouldn’t even be able to devote that much time in such an emergency. While it’s certainly possible that I might have hit on the right thing to say if I’d worked on it even longer, my focus at that time was arousing her so that she could safely leave my office, as the behavior occurred at the end of the session. This goal—to have her leave my office—probably came through in my tone and interventions, despite the reassurances that I tried to offer. I was mystified about the exact source of the shutdown, and reassurance alone wasn’t effective. Perhaps unconsciously, Trina was saying that her only safety was in my office, and she couldn’t “leave,” grow up, or achieve adulthood. Thus, my own goal to have her leave my office was incompatible with her goals.
Episodes of unpredictable shutdown, sometimes seen as psychogenic seizures, are sufficient for hospitalization since they can be dangerous. Young people in this state can fall down and hit their heads or not be responsive to the outside world for hours at a time. The question of whether Trina was a treatable inpatient or outpatient was debatable, in that the doctor in the ER thought she was eligible for admission the night before, having witnessed the shutdown state. Had she not been able to use the episode to gain further self-knowledge and increase control, the episode could have been classified as “unpredictable,” and an argument made that this behavior was too dangerous for her to be treated as an outpatient. Realistically, however, had she not been able to get to the bottom of this episode the next day, but seemed to be trying, I most likely would have made another “deal” with her to keep her out of the hospital.
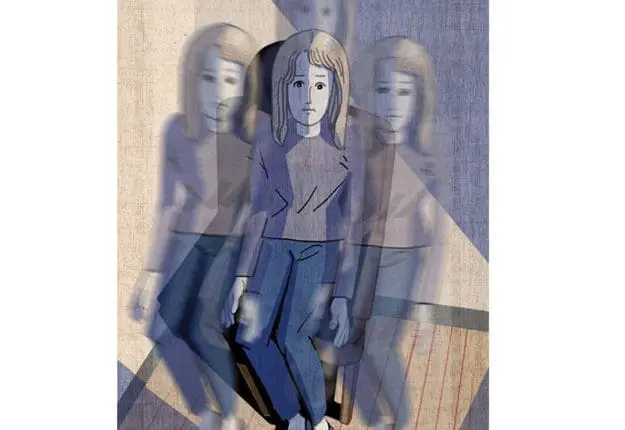
Illustration © Sally Wern Comport
Joyanna Silberg
Joyanna Silberg, PhD, consulting psychologist at Sheppard Pratt Health System, is the author of The Child Survivor: Healing Developmental Trauma and Dissociation. She’s the past president of the International Society for the Study of Trauma and Dissociation.
David Crenshaw
David A. Crenshaw, PhD, ABPP, is Clinical Director of the Children’s Home of Poughkeepsie. He is Past-President of the New York Association for Play Therapy, a Board-Certified Clinical Psychologist; a Fellow of the American Psychological Association, a Fellow of the Division of Child and Adolescent Psychology, a Fellow of the Academy of Clinical Psychology, and a Registered Play Therapy Supervisor. He was honored with the Excellence in Psychology Award in 2009 and has received two Lifetime Achievement Awards: in 2012 by the Hudson Valley Psychological Association, and in 2018 by the NY Association for Play Therapy. He is the author/editor/co-editor of 17 books, over 100 book chapters, and journal articles on child aggression, play therapy and child trauma, his books co-edited with Cathy Malchiodi are What to Do When Children Clam-Up in Psychotherapy and a book co-written with Eliana Gil titled Termination Challenges in Child Psychotherapy.