No diagnosis conjures up stigma quite like borderline personality disorder (BPD). Early in my career, while working in psychiatric hospitals, I was warned that BPD was very resistant to treatment and the best we could do was set firm boundaries with these patients and resist their attempts to manipulate us. Admittedly, it’s tempting to have a clear label for difficult clients who present with swift changes in mood, impulsive behaviors, and an uncanny ability to expose our vulnerabilities. However, many clinicians today believe we’ve unfairly pathologized people some call “borderlines,” rather than acknowledge our failure to do a better job of addressing the attachment issues underlying their struggles.
While therapy approaches like Marsha Linehan’s dialectical behavior therapy have provided guidelines for teaching these clients coping skills, research indicates attachment trauma plays a major role in the development of BPD. Indeed, when I began to think of BPD as being a form of anxious or disorganized attachment, instead of a terrifying mental illness, treating it became easier. More importantly, my clients got better.
Leslie was one of the tormented souls who taught me this lesson. Even though she was 30 years old, she looked like a teenager the day she shuffled into my office, wearing baggy jeans and a huge Hello Kitty sweatshirt that swallowed her lithe, 90-pound, 5’ 2” frame. Her pale blue eyes peeked out timidly beneath her curly red hair. She whispered, “My husband is in your waiting room. He’s going to try to listen in, so we have to talk quietly. He and my psychologist are trying to commit me to an inpatient unit. I need you to convince them I’m not crazy.”
Double Binds
My breath halted as I contemplated how to avoid being pulled into this thorny conflict, yet her eyes were pleading with me for help. Controlling my own fear, I took a deep breath and responded, “My goodness, that sounds like a scary situation for you. What makes your psychologist and husband think you need inpatient treatment?”
Leslie’s eyes narrowed as she glanced to the side and said, “They think I have an eating disorder because I can’t eat. I want to eat, but I can’t swallow. My throat feels like it’s swollen, and I can’t get anything down without choking. The doctors say there’s nothing wrong with me. I heard you did hypnosis and thought maybe you could hypnotize me and get my throat to relax—or at least tell my family and psychologist I’m not crazy.”
“Who’s your psychologist?” I asked.
Leslie crossed her arms. “I’m not ready to share that information,” she shot back. “I need you to hear my side of the story. Sheesh! I’d hoped you’d be different.”
This stung, but she was right. While I didn’t feel comfortable treating her if she was seeing another psychologist—and I was concerned that person thought her issues warranted hospitalization—in my effort to protect myself, I’d invalidated her experience. I swallowed my pride and said, “You’re right. That must have sounded insensitive to you. Tell me how this all started. I want to understand it from your perspective.”
Leslie had started having digestive problems when she was 15. Her symptoms included difficulty swallowing, acid reflux, and food sensitivities. Her parents thought she was feigning these symptoms and didn’t take her seriously until her weight became dangerously low and she fainted at school from hunger. The doctors suggested she had an eating disorder and recommended psychiatric treatment. Her parents took this as confirmation that Leslie was just acting out for attention. Rather than help her, they told her to “get over it.”
Leslie said she could manage for a while by forcing herself to swallow down meals in spite of the reflux. But she still had episodes when the pain and gagging reflexes would erupt to the point she couldn’t eat. The most recent episode began six months ago—right after her husband asked for a divorce.
“Oh goodness,” I said. “That must have been terribly painful. No wonder you’ve been feeling sick.”
Her lips quivered as she sobbed, “I vacillate between hating myself and then hating everybody else. Sometimes I cut myself when I can’t take the pain inside. I’m not trying to kill myself. I just want someone to listen to me. I just want someone to believe me.”
Leslie sniffed, grabbed several tissues, and continued, “When I started getting sick again, my husband said he wouldn’t leave. Now he wants to put me away. I don’t know what to do.”
We talked about the problems in her marriage. She loved her husband but believed he often dismissed her feelings. When she complained about this, he accused her of being too needy. Leslie said her family had done the same thing when she was growing up. She said, “I learned to hide my feelings from my family because showing any vulnerability would leave me open to more attacks. So I buried my emotions deep down inside. But when it gets to be too much, I get sick. I don’t know how to stop it.”
Seeing the emotional pain she was in, I offered to show her an imagery exercise that could help her soothe herself until we could find a better solution to her problems. I explained to her that our bodies tense up under stress and that stress hormones can impact our digestive tracks and contribute to the physiological issues she was experiencing. I reassured her that this didn’t mean her physical complaints weren’t real, but that using this self-soothing technique might help calm them down. To start, I suggested she imagine how she wanted her body to feel instead of how it had been feeling.
Leslie replied, “I want to feel like I have more space in my throat and to feel like things can flow more smoothly, whether it’s food going down or my words coming out.”
Impressed with her insight, I cheered, “That’s perfect! Now let your mind show you a symbolic image that could represent your mind and body working that way. The emotional part of our brain doesn’t speak in words. It responds better to pictures, or music, or movement. What comes to mind when you imagine space, smoothness, openness, flowing?”
Leslie closed her eyes. “I see a waterfall.”
“Beautiful! Now take a deep breath and imagine that waterfall. Perhaps you can imagine what it would be like to be the waterfall with things flowing smoothly and naturally, soothing your body, clearing out the tension, expressing your authentic strength and beauty.”
Leslie closed her eyes, breathing smoothly and rhythmically. Her shoulders relaxed and her facial features softened. After several minutes in this reverie, she opened her eyes and said, “That felt nice. This is what I want. Would you be willing to see me as a client?”
While I was open to seeing her, I told her I couldn’t ethically see her as a client until I cleared it with her psychologist. She was worried that her psychologist might be angry or say bad things about her to me. I reassured her that I understood her side of the story and could work through any misunderstandings, if they arose. She reasoned it was worth the risk and signed a release for me to speak to her psychologist, Dr. Z.
Manipulation or Cry for Help?
It turned out that Dr. Z was a colleague I knew well, who specialized in eating disorders. She returned my call promptly, saying, “Ah, I see Leslie’s attempting to triangulate you into this. If you want to see her, that’s fine with me. Honestly, I don’t know what else to do. She’s a classic borderline personality, and I’m not sure I’m helping her.”
When I asked if she thought Leslie needed to be hospitalized for her eating disorder, Dr. Z said, “No. She’s underweight, but not to the point of needing hospitalization yet. Clearly, she has disordered eating, but I think it’s a symptom of her personality disorder. She uses somatic complaints to manipulate her family. I warned her that if she didn’t stop, she could wind up in the hospital. I thought that would motivate her, but I guess it just made her feel more hopeless.”
Dr. Z. seemed to be feeling hopeless, too. Although the BPD diagnosis was meant to help clinicians select appropriate treatment interventions, too often it blinds us from seeing the source of our client’s pain. Rather than blame BPD for Leslie’s behavior, I wondered aloud, “Why does she feel she has to manipulate her family to get her needs met?”
Dr. Z. replied, “Well, they can be dismissive of her, but that’s because she’s cried wolf so many times.” I wasn’t satisfied with this explanation. Even though I realized this would be a challenging case, I felt compassion for Leslie and agreed to take her as a client.
At our next session, she cheerfully bounced into my office and exclaimed, “Guess what? I’ve been using that waterfall imagery you taught me and it’s helping. I gained two pounds this week! I knew you were the right therapist for me.”
Encouraged but worried Leslie was idealizing me, I said, “You’re the one who used the tool and made it happen. Be sure to give yourself credit, Leslie.”
“Give myself credit. That’s hard for me to do. My family never would,” she mumbled. While her family seemed “normal” on the outside, she continued, growing up she’d felt bullied and picked on by her parents and older brother. She was a shy, sensitive child, who loved animals, music, and poetry, and she recalled feeling emotions more intensely than others from a very young age.
When she felt joy, she’d get energized and squeal with excitement. But rather than sharing her joy, her family would tease her—or worse, accuse her of being annoying. When she felt sad, her family would shame her with comments about how good she had it, telling her to stop feeling sorry for herself. When she was angry, they’d tell her she was acting spoiled and was lucky they didn’t believe in spanking, or they’d “knock her into next week.”
Leslie had resigned herself to this misunderstood existence until one afternoon, when using her dad’s computer, she saw an email suggesting he was having an affair and planned to leave his family. She immediately told her mom, who didn’t believe her. Her dad said she’d imagined it. She was 15 years old. “That’s when the nausea, reflux, and self-mutilation really kicked in,” she noted. “My dad decided to stay when I got sick, but a few years later, he did leave us for that other woman. I haven’t talked to him since.”
Leslie and I explored the connection between her gastrointestinal flare-ups, urges to cut herself, and experiences of feeling invalidated or abandoned by her family and husband. She agreed there was a connection, but protested, “Listen, I’m not doing this on purpose for attention! I hate feeling like this.”
Reassuring her that I believed her, I validated that the stress of these losses could certainly exacerbate feelings of emptiness and internal pain. I suggested that the body may communicate what we don’t feel safe expressing verbally. My intention was to make it safe for her to talk with me about her pain instead of swallowing her feelings. But she misinterpreted my intention and shot me a suspicious glance. “Dr. Z. thinks I have BPD. Do you agree with that?”
Her question gave me pause. While her experiences fit with Marsha Linehan’s biosocial theory of BPD—that people who develop it usually have an inherited tendency toward emotional sensitivity and impulsivity coupled with a family environment that invalidates the child’s emotions or reinforces negative responses—when I’d tried discussing BPD as a possible diagnosis with previous clients in hopes that it would give them a way to understand their symptoms, it hadn’t really helped. They usually reacted with feelings of shame, anger, and more hopelessness.
This time I tried something different. “You know I’ve never found that diagnosis helpful. I think it’s more accurate to say you’ve been experiencing what we’d all feel when we don’t feel validated and understood by our family, or have a loss in a relationship.”
I explained to Leslie that humans, like all mammals, are biologically wired to attach to a pack for safety and survival. When we don’t feel safe and connected to our pack, or family, our nervous systems can react as if there’s a threat to our survival. This translates into the body releasing lots of stress hormones, like adrenaline and cortisol, which can wreak havoc on the digestive system. In addition, it can cause our brains to be ultrasensitive to the slightest hint someone could harm, abandon, or reject us. Moreover, if our brain and body learn that making us sick gets our family to be more caring, that can trigger those same reactions any time we feel misunderstood or abandoned.
I reassured Leslie that her brain and body were not broken, but simply attempting to get her emotional needs met in a way that had worked in the past. The solution was to update those neuropathways by helping her find better ways to feel safe and connected.
Leslie nodded, “That makes more sense than anything I’ve heard. How do we do that?”
“First,” I said, “I’m going to do my best to attune to what you need emotionally and help you feel validated, understood, and supported. When someone genuinely feels these things, they can discover how to soothe and take care of themselves in a different way. But there are going to be times I make mistakes, or say something that’s hard to hear. When that happens, I ask that you be patient as we figure out how to work through any misunderstandings. I’m learning too, and, though I mean well, I’m not perfect.”
“I’ll try to cut you some slack,” Leslie teased, “as long as you cut me some too.”
“Second,” I continued, “we can use a process called memory reconsolidation to update negative messages you may have learned about yourself or others. There will be times we may revisit painful moments from your life to help your emotional brain process them in a more secure and grounded way. For example, we may use imagery, like we did with the waterfall, to help you access resilience and rescript those memories. We may show your emotional brain that you were not a needy, overreactive kid, but that your parents were sorely lacking in the knowledge and skills they needed to guide and comfort a creative, sensitive child. I won’t be making excuses for your family but helping you see that their mistakes were coming from their own emotional immaturity and ignorance, so it feels less personal and threatening.”
Leslie cocked her head to the side, “I liked the imagery and am open to trying that.”
“Last,” I said, “I’ll be teaching you skills for understanding and managing your emotions, communicating your feelings, and handling conflicts more calmly. Many people don’t learn these skills. They’re not generally taught to us by our schools or families.”
“How long is this going to take?” Leslie asked.
“I don’t know. You strike me as being bright and motivated, so I think you’ll pick it up quickly. But you’re dealing with several major stressors right now, so we’ll likely alternate between sessions where I simply support you and help you make sense of your reactions, and sessions that focus on healing old memories and building new skills.”
And so it began.

Leslie and I worked together for five years. During most of our sessions, I saw my job as staying as attuned and present as possible while she gave voice to her experience. There were plenty of times I doubted myself and wondered if I was enabling her by not challenging her enough. But within six months, she’d gained 30 pounds and was back to a normal weight. She even began to look more mature, ditching the Hello Kitty clothes for outfits considered fashionable for a woman in her 30s.
Her marriage didn’t last, and she regressed dramatically while going through the divorce. She stalked her husband and attempted to manipulate him with threats of suicide and other tactics employing fear, guilt, and obligation. In the past, I would’ve been tempted to hospitalize her, but I saw her reactions as similar to the way an immature 15-year-old might react to a breakup, and I used interventions that often worked with adolescents, like journaling, making music playlists, role-playing, and using humor. I continued to express compassionate curiosity as we explored which behaviors seemed to pull people closer to her versus those that pushed people away. I was careful not to portray her husband as the “bad guy” but someone who lacked the emotional sensitivity skills she might want in a partner. I helped her explore what a healthier relationship might look like.
In the last years of our work together, she joined a church, began to write songs, and was shocked when her choir wanted to sing them at a service. Her mother even began to attend church with her, and they started to forge a more caring, close relationship. Leslie’s transformation didn’t happen overnight; there were many setbacks, conflicts, and challenges along the way. But whatever else might shift in the therapy, for me one thing remained unchanged: Leslie was always a person, never a diagnostic category.
CASE COMMENTARY
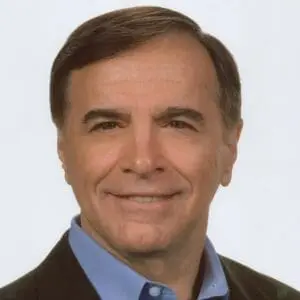
By Steven Stosny
This case highlights a major impediment to successful treatment. For many clinicians and most laypeople, BPD has become little more than a negative label. (I’ve heard colleagues use it as a slur.) As Courtney Armstrong points out, the diagnosis carries built-in excuses for our failures and reinforcement of our biases.
To her credit, Armstrong treats people, not diagnoses. She keeps her head and heart open under the fire of a desperate client whose history of pained relationships leads her to almost dare the therapist to help her. Rather than use pejorative terms like manipulation, Armstrong addresses the pain that causes Leslie’s symptomatic behavior, using a growth-oriented approach to self-regulation skills.
This is especially important with Leslie, who’d otherwise interpret the need to learn self-regulation as more evidence of her perceived defects. Above all, Armstrong’s patience and compassion with Leslie make it possible for her to bring patience and compassion to her own relationships.
The foundation of Armstrong’s intervention is validation, something we must do for clients who are unable to self-validate. But it’s also important to foster perspective-taking, which is the only thing that breaks the self-obsession of intense feelings and reduces the sense of isolation they perpetuate. Compassion for Leslie is crucial to her recovery, but it’s her compassion for others that ultimately heals her.
Validation and perspective-taking for Leslie would come in small steps and look something like this: “My husband dismisses my feelings.”
“God, that feels awful. Everybody feels bad when a loved one dismisses their feelings.”
Leslie would talk more about how bad it feels, all of which would be validated. Then the therapist might say, “I wonder what’s going on inside him, what makes him feel that he’s not strong enough to give you emotional support? He probably would like to, what do you think?”
Instead of a sign that she’s too needy, her husband’s dismissiveness now means that he, too, feels inadequate, unlovable, and a failure as a partner. She can feel empowered by her compassion for him. And, of course, she’s likelier to get compassion from him when she’s able to see his perspective alongside her own.
Practicing validation and perspective-taking with a client like Leslie requires a kind of emotional stamina that I don’t always have. And that’s why I admire the steady focus and sustained empathy that enables Armstrong to move beyond just treating a diagnosis to offering Leslie a powerful experience of healing.
Courtney Armstrong
Courtney Armstrong, LPC, MHSP, is a Board Certified Fellow in Clinical Hypnotherapy and has trained thousands of mental health professionals in creative, brain-based strategies for healing trauma. She’s a bestselling author of the book, The Therapeutic “Aha!”: 10 Strategies for Getting Clients Unstuck and Transforming Traumatic Grief and is the owner/director of Tamarisk: A Center for Mind-Body Therapy in the state of Tennessee.
Steven Stosny
Steven Stosny, Ph.D. is a well-known therapist and author of many books and articles. He’s appeared on all the major networks and national radio shows, most of the major newspapers and magazines. He has taught at the University of Maryland. His blog on PsychologyToday.com has more than 21 million views.