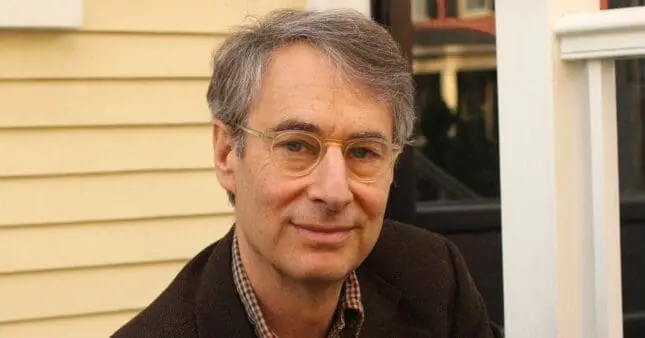
Ordinarily Well: The Case for Antidepressants
by Peter Kramer
Farrar, Straus & Giroux. 308 pages.
9780374280673
If you listen to Peter Kramer—distinguished psychiatrist and author of the 1993 bestseller Listening to Prozac, among other well-regarded books—SSRIs aren’t mere placebos oversold by Big Pharma to an easily gulled public, as some critics continue to charge. On the contrary, in his latest book, Ordinarily Well: The Case for Antidepressants, Kramer argues passionately that these medications represent the best, most effective tool we have to fight the bleakness of depression.
Part of the evidence, he contends, is the almost complete absence of cases today exhibiting the most severe end-of-the-line depression that he encountered regularly in hospital wards during his medical training in Boston in the late 1970s. These patients, he writes, were “thin, immobile suffering souls, prematurely aged,” almost mute, depleted of all energy. Although antidepressants like imipramine had been available since the 1950s, the doctors with whom Kramer trained (many of them Freudians) scorned them as an unnecessary crutch at best, and an impediment to the workings of the unconscious at worst. Thus, when talk therapy alone didn’t work, patients were left to grit it out on their own—which too often meant continuing to suffer and deteriorate into ever deeper despair.
Today, these types of cases are so rare that most clinicians can count their experiences with them on one hand. The reason, Kramer and many of his colleagues believe, is that depression is now routinely nipped in the bud when primary care doctors or psychiatrists prescribe SSRIs before the disease can worsen into ever more severe recurrent episodes and ultimately reach that end-stage, emotionally paralyzing state. The result has been transformative, he writes: “On the model of cancer, with depression we have turned terminal cases into chronic ones.” Judging from this alone, SSRIs have made a giant impact in relieving human suffering. These days, he says, for a contemporary practitioner to let depression fester without trying medication is tantamount to malpractice.
That’s a strong message, and Kramer’s full endorsement of antidepressants is news for several reasons. In his previous books, his attitude toward antidepressants in general and SSRIs in particular can best be described as an ambivalent “yes, but.” In fact, his title Ordinarily Well is a play on the phrase “better than well,” which he coined in Listening to Prozac to describe how SSRIs often make people with depression feel after their symptoms lift. In turn, it caused him to wonder if the meds were allowing his patients to become their “true” selves, functioning without the oppressive cloud of depression, or if they were experiencing the result of what he dubbed “cosmetic psychopharmacology,” in which meds could be used to improve a person’s inner disposition. If it’s the latter, would SSRIs be overprescribed to favor more socially accepted “upbeat” personalities over more prickly or introverted types? These phrases stuck, becoming part of the lexicon of the ongoing debate about the use of antidepressants.
In his latest book, Kramer writes, he’s grateful for the help these medications bring his patients, yet at the same time he’s still wary of the dangers of overprescribing. He also remains a strong believer in the benefits of talk therapy, and treats the majority of the people who come to him with both medication and psychotherapy. Indeed, he’s found that psychotherapy tends to become more effective once antidepressants begin to ease the symptoms of oppressive mood and anxiety that cloud coherent thinking. But he now fears that his previous reservations have been misunderstood, even overblown, helping foster a growing wave of opposition to antidepressants.
Over the past 10 to 15 years, we’ve seen a series of books challenging what their authors consider to be inflated claims in favor of SSRIs. These books include David Healy’s Let Them Eat Prozac: The Unhealthy Relationship between the Pharmaceutical Companies and Depression (2004), Charles Barber’s Comfortably Numb: How Psychiatry Is Medicating a Nation (2008), Irving Kirsch’s The Emperor’s New Drugs: Exploding the Antidepressant Myth (2010), and Robert Whitaker’s Anatomy of an Epidemic: Psychiatric Drugs and the Astonishing Rise of Mental Illness in America (2011). Only slowly, as these books appeared and amid the growing trend to distrust doctors and medications in general (witness the widespread antivaccine movement), did Kramer begin worrying in earnest about the potential public health consequences of a tide turning against SSRIs: caregivers declining to prescribe, and clients refusing to take, the very medications most likely to help them. Would we see the return of the bad old pre-SSRI days, with increased numbers of clients suffering from end-stage paralyzing depression?
This state of affairs hit close to home for Kramer when, in 2011, one of his best friends suffered a stroke. Kramer urged the neurologist treating his friend to consider prescribing an SSRI, which several studies had shown to be beneficial, not just for preventing depression (a common sequel in stroke victims), but also for preserving the ability to think clearly—a benefit that improves quality of life and increased survival time. The neurologist was skeptical, however. Not only had he read news reports questioning the usefulness of SSRIs except for the most severe depression, but even worse, he didn’t seem to be aware of the medical literature about the neurological benefits of antidepressants. (The neurologist ultimately was convinced, and Kramer’s friend did improve as a result.)
Kramer’s decision to challenge the increasingly critical view of psychopharmacology was further reinforced when he found himself drawn into a public argument with Marcia Angell, the influential physician and former editor of The New England Journal of Medicine, who’d dismissed antidepressants as useless placebos in a widely read article in The New York Review of Books and whose view Kramer subsequently tried to rebut in his own article in The New York Times. Angell, as blunt a critic of pharmaceutical companies as she is a strong advocate of evidence-based medicine, cited research that Kramer believed to be based on faulty assumptions. Angell, in turn, faulted Kramer for being overly dependent on anecdotes from his clinical practice.
Ordinarily Well asks, first and foremost, do antidepressants work? To that, Kramer cites extensive research from the 1980s on to answer, unreservedly, yes, the majority of people suffering from depression do fare better on antidepressants than on placebo pills. As for unpublished negative studies, including those by pharmaceutical companies, he writes, “Even looking at failed and unsuccessful trials, sweeping in all the data, if you limit your attention to core symptoms, you find that antidepressants perform at acceptable levels.” He also reports on potential side effects associated with long-term use of some antidepressants, including increased rate of cataract formation, an effect on the calcium absorption of bones, and even possible changes in electrical conduction in the heart.
Chapter by chapter, Kramer offers a thorough and painstaking reading of a large number of studies on the treatment of depression. To help us make sense of them, he explains the designs and ideas behind different types of studies and why those differences can make them more—or less—reliable than they may at first seem. For instance, evidence-based medicine, as advocated by Marcia Angell, seeks to encourage practitioners to follow the conclusions gleaned from study outcomes, rather than what they’ve learned from their clinical experience. But, as Kramer tells us, a host of factors can affect the outcomes of the studies and their possible interpretations. For instance, most studies underestimate the effect of SSRIs because they’re generally limited to dispensing to every subject receiving a medication the same dosage, over the same duration of time. That kind of cookie-cutter approach is the antithesis of clinical practice, Kramer asserts, in which psychiatrists work to match each patient with the right medication and dosage, while remaining flexible about making changes as the course of treatment continues.
Kramer also finds that meta-analyses, the type of study favored by Kirsch and others, are often problematic. A meta-analysis is a statistical tool that combines and integrates the findings of a large number of studies with the aim of reaching a more accurate conclusion than any one of the single studies by themselves could provide. That means that the quality of the meta-analysis will depend heavily on, first, the quality of the individual studies included, and second, on the similarity of the subjects and of the questions each study explores. As a result of such matching (or not), meta-analyses can be open to differing interpretations, cherry-picking, and the weighting of some results more heavily than others.
As he spells out all these points, Kramer’s prose can be dense with statistics, technical in its explanations of such matters as effect sizes, the nature of randomness in trials, and other complex methodological issues used in the design and analysis of research studies. But this context is necessary for understanding the claims both for and against the effectiveness of antidepressants. In fact, in Kramer’s view, the question isn’t if antidepressants work (in his clinical experience and his reading of the literature, they do): instead, the debate “is over the magnitude of the effect size”—in other words, how much of a therapeutic impact they have.
The book is most compelling when Kramer recounts case studies of his own patients and how they fared without—and with—antidepressants, and especially the ways in which the artful use of pharmacology has aided the process of psychotherapy. In the final chapter, he writes, “Denying the efficacy of antidepressants may begin well enough, with a love of psychotherapy and a respect for human complexity.” But he believes this denial discounts the benefits that have been proven and can result in withholding those benefits from suffering patients. Listening to his patients, he emphasizes, has made him more mindful of those benefits. “Over time in session, I’ve heard repeatedly how depression dampens responses to love and beauty. When medication works, the world does its bit. Patients are freed to notice what’s precious in their lives.” Meanwhile, the debate over SSRIs continues. Regardless of your own position, Kramer’s voice is well worth hearing out.
Photo © Matthew Kramer
Diane Cole
Diane Cole is the author of the memoir After Great Pain: A New Life Emerges and writes for The Wall Street Journal and many other publications.