As a therapist who specializes in working with eating disorders, I often see people in my office who struggle with issues around restricting their food intake, overexercising, or engaging in purging behaviors. Although binge eating disorder (BED) is the most common type of eating disorder—with a 3.5 percent prevalence rate in the United States, compared to 0.9 for anorexia and 1.5 for bulimia—many people suffering with it don’t get the help they need because of their embarrassment about their bodies and eating habits. They often have long histories of disordered eating, multiple unsuccessful diets, and shameful interactions with medical professionals. Many of them avoid seeing therapists for fear of more shame and more useless advice to just stop eating.
Because people with BED have higher rates of depression, anxiety, and addictive behavior, many therapists overlook the symptoms of BED, which include recurrent episodes of overeating, even when not physically hungry, a sense of lack of control during these episodes, eating more rapidly than normal, feeling uncomfortably full, and feeling guilt after overeating. Research suggests that 30 to 40 percent of individuals seeking weight-loss treatment could be diagnosed with BED; however, not all larger-sized individuals have BED, nor do all of those who have BED necessarily have larger body sizes.
Despite its prevalence, BED didn’t get its own category in the DSM until 2013, meaning that it’s no longer grouped into the “other specified” category and has been defined as a condition requiring specific treatment. Of course, the approach to treating it and related concerns is similar to other eating-disorder work, but we need to be especially vigilant about addressing issues of self-agency and keeping their focus more on wellness than weight, even though societal, family, and often medical pressures can run counter to that approach. In my work with Diane, these pressures were so strong that we had to recommit to a focus on emotional well-being several times throughout treatment.
Approaching Food Differently
In our first session, Diane, a 34-year-old graphic designer, let out a sigh of relief as she saw the couch in my office and realized she wouldn’t have to struggle to fit into one of the chairs. She began boldly, “I’ve gained about 200 pounds since college. I’m now 350 pounds and need to do something about this.” She explained how she’d tried dozens of diets and hadn’t been able to stick with any of them long enough to make any difference. Her medical doctor had brought up the idea of gastric bypass surgery several times, but Diane had read about the risks of this procedure and wanted to try something else.
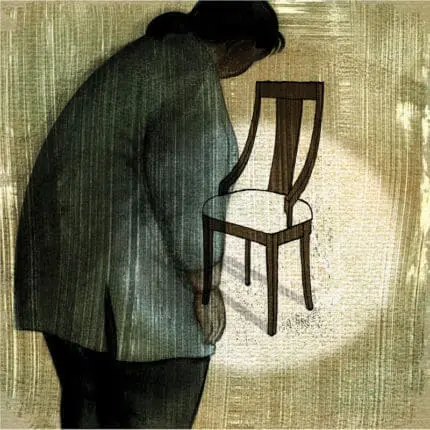
Some of the struggles she described highlighted her deep shame about her body size and eating. She was embarrassed to sit at a table in a restaurant and was self-conscious about filling up her shopping cart at the grocery store, so she usually ended up getting most of her meals by frequenting drive-throughs or ordering takeout to her home. She ate quickly, in secret, with guilt.
Diane recounted some of the details of plans she’d been prescribed over the years—more than 20 different approaches that left her feeling like a failure because she could never stick with them. “Which diet do you recommend?” she asked tentatively.
“I don’t think you need another diet,” I told her. “You may be thinking you’ve failed at dieting, but it’s the diets that have failed, because they don’t work long-term. I do, however, believe that shifting your relationship with eating would be useful. I also believe we might need to do some work on underlying issues that may be contributing to some of the patterns.”
I shared with her how I approach eating disorders from a non-diet perspective and suggested that we work on health from a broader perspective. I explained how most people find they have more success in shifting specific behaviors than in focusing on a specific target weight. As we talked about this new way of approaching the process, she was intrigued but a bit anxious. She liked the idea of focusing less on weight, but was such a people-pleaser that doing something so antithetical to what everyone expected of her, which was simply for her to drop numbers from the scale, created some internal tension. We went on to discuss some of her other anxiety issues tied to eating, such as experiencing so much worry over what to choose from a menu that she often ordered multiple entrees to make sure she liked what she got.
When Diane returned for her second session, I asked my typical question of whether anything from our first session was unclear or striking. What stuck with her the most, she said, was when I’d told her, “You have an eating disorder, not a character flaw.” She’d felt, as do so many with BED, that her overeating was a willpower issue and had never considered that it might be much more than that. She’d come to feel excited about focusing on improved health and overall self-care. “I see now how dieting was part of what triggered my binge eating,” she added. “It became more damaging than helpful.”
“You got it, Diane!” I said. “I’m pleased that you heard that takeaway message so clearly. I get the feeling you’re not used to treating yourself with compassion, but I sense that you made some space for considering that as a possibility. Thank you. I’m excited for us to begin the journey of figuring this out together.” I felt enthusiastic, but was mindful of choosing my words carefully so as not to suggest this was a simple fix. This journey is difficult, long, and unpredictable. Diane would likely have ups and downs in her progress, while continuing to feel pressure to do the quick fix of diet or surgery.
Part of our work over the next few months would be psychoeducational, challenging Diane’s many distorted ideas about eating and her body. She assumed, for instance, that her larger-sized body meant she’d be able to sustain herself on very little food each day, something she’d tried repeatedly only to find herself ravenously hungry each evening. She also assumed that when she did eat, it should only be low-fat, low-carb, diet foods, and this further left her feeling deprived and more ravenous. I talked about basic biological needs and introduced the HAES (Health At Every Size) approach. We also talked about fundamental behavior changes, such as slowing down her eating and chewing more mindfully. Eventually, she agreed to experimenting with the steps of mindful eating in our sessions, so I could help her find ways to tune in and allow her meals to be more satisfying, thereby decreasing her excessive cravings.
“I don’t think I ever really tasted all the flavors of the eggplant curry I order so often from the place down the street,” she told me one day. “When I got it last Friday, I did inhale some of it, but then I remembered to slow down, breathe, and noticed more about the textures and the spices.” Diane paused and added with a smile, “I even ended up putting some of it into the refrigerator for lunch the next day. I’ve never done that before.”
“Diane,” I grinned, “that’s fantastic on so many levels—doing a U-turn midmeal, refocusing on the skills you’ve been learning, and even fighting some old urges to eat everything even when you’re full. Wonderful examples of progress!”
In working on the eating changes, we slowly uncovered other anxiety-based habits that had been contributing to her BED. She had some symmetry superstitions that led to her feeling that a pizza had to be completely gone or exactly half gone, and some obsessions around certain numbers, such as feeling she needed to plate items in multiples of five. We approached each of these through practicing exposure and engaging in doing the opposite of what her anxiety commanded. After a while, she could catch herself more often when anxiety threw a rule at her, frequently saying to me, “I remembered last night not to believe everything I think.”
I was pleased about the many behavioral and mindset changes Diane was making, but I knew they likely wouldn’t lead to quick weight loss. And as I suspected, her excitement about these changes waned whenever the weigh-ins at her doctor’s office indicated only one or two pounds of weight loss. At these points, we needed to review the goals of our broader wellness work—which eventually led Diane to take my recommendation of seeing a specialized nutritionist. We discussed how weight maintenance is actually progress, as it’s different from the monthly weight gain that had been the case for years. “Remember to zoom out for better perspective,” I regularly reminded her.
Coping with Complications
One day, Diane appeared in my office looking sullen, with her leg in a brace that seemed to do little to ease her pain as she hobbled over to the couch. Earlier that week, she’d twisted her knee while climbing the stairs to her apartment. Her doctor, who’d been monitoring her for prediabetic symptoms, told her she’d need to wear the brace for more than a month, making movement and getting dressed even more laborious.
“I know I wouldn’t get hurt so easily if I weren’t carrying around so much extra weight,” she muttered. “And Aunt Shelly is always worrying about me dropping dead of a heart attack.” I heard a lot of self-blame in her voice, which turned to frustration as she recounted how her doctor had again brought up bariatric surgery. Diane remained opposed to it. “I know I have to keep working on this if I want to live a good life,” she asserted, tearing up a little. “But I think that surgery is too risky.”
It wasn’t my role to choose whether she should have the surgery, but she seemed relieved that I was supportive of our staying on course in our work together and to know that I was willing to confer regularly with her physician. Weight-loss surgery may be faster than the time-consuming process of changing habits and of uncovering deeply entrenched beliefs, but psychological treatment for BED also has long-term benefits, which Diane was just beginning to understand. “You’ve already started the important work of improving your health by honoring rather than punishing your body,” I encouraged her. “You’ve been starting to adopt more habits for the sake of health, rather than getting fixated on a number on a scale. Heck, even you taking the stairs more often is part of that—it was just unfortunate that you got this knee injury.”
Diane nodded, but her eyes remained downcast. I worried the knee injury would cause her to feel more hopeless and lapse back to self-punishment, which often involved overeating. So we focused on maintaining her eating changes while finding other coping tools to manage the difficult times, such as adding more compassionate self-talk and mindful breathing to her daily routine. We addressed other anxiety triggers, such as worries about being passed up for a promotion on account of weight stigma, or feeling insecure about attending social events without properly fitting elegant clothing. I made sure Diane felt validated in these frustrations, which are common for larger-sized individuals, pointing her toward authors who write eloquently about this topic, such as Geneen Roth, Roxane Gay, Michelle May, and Linda Bacon.
Although these authors inspired her, Diane still admitted that she was too scared to ask her manager for a chair without arms at a meeting. So we focused on specific strategizing, such as assertiveness role-plays. “If your coworker were in a wheelchair due to a broken leg, wouldn’t you think it reasonable that the meeting be held in a wheelchair-accessible location with elevators?” I asked her. “You deserve to ask for what you need. Let’s practice again where I pretend to be your boss in a bad mood.” Diane wasn’t accustomed to asking for what she needed or even feeling justified to ask for something she felt was her fault. By practicing this new boundary-setting language together, she worked on her sense of confidence and ability to shed the guilt she was carrying about the weight. Eventually, these role-plays even helped her set more boundaries with the parts of herself that wanted to binge.
Making Other Connections
After a few months, Diane admitted at the start of one session, “I had another binge episode last night. I ordered all the stuff I used to and ate it all, even though I was completely stuffed halfway through. I’d had some stressful meetings at work, and I probably didn’t eat enough during the day, but this is the opposite of my goals! Will this ever change?” she asked dejectedly.
This type of setback is common but still discouraging for both the client and the therapist. I took a deep breath, and reminded both of us that the recovery path isn’t straight or smooth. “The fact that it’s been over a month since the last significant binge episode is a huge change, Diane!” I countered. “And I’m impressed that you’re aware of the vulnerabilities, such as stress and being hungry during the day, that probably lead to it. This sounds like the kind of insight you’ve been translating into behavioral changes lately. Remember last week when you noticed getting frustrated at your boss and went outside with your headphones instead of binging on the vending machine snacks? And remember the week before when you noticed you were very hungry as you were driving home from work and planned for a predinner appetizer so that you weren’t starving while cooking the dinner you’d planned? Those are examples of progress in approaching eating and stress differently.”
“I know,” she replied, pulling on a loose strand of hair from her ponytail, “but I’m disappointed in myself. I understand now what you’ve been saying about ‘normative eating’ and how I have to separate out physical from emotional hunger, so why does this keep happening?”
There isn’t one specific cause of BED, but research indicates several risk factors, such as genetics, dieting at an early age, affective disorders, experiences of weight bullying, significant family problems, and trauma. Diane, unfortunately, had a number of risk factors in her history, and to help her to take on less guilt over them, we focused much of our work on their impact. During one particularly reflective session, she even identified some ambivalence about losing weight related to her father, who often told her when she was growing up that he wanted her to be thinner. She realized that some of the worry about changing her patterns now could still be coming from a rebellious reaction to his attempt to control her.
“If I lose the weight now, he might think he was right all along,” she said, “and I don’t want him to get any credit for that. He’s an asshole, and I don’t want him to gloat.” By acknowledging this resentment more openly, she was able to create more boundaries around time spent with him, anticipate the anxiety-management skills she could use around him, and create ways to take all the credit for her progress.
Outward Exploration
At the start of one rainy-day session, Diane wondered aloud, “What if I lose more weight but am still unhappy?” She now knew weight loss was a complex issue and didn’t lead to automatic contentedness.
“Sounds like you might be scared of creating a life you want? Or you’re worrying you aren’t worthy of it?” I asked gently. Tears sprung to her eyes. We reflected on the ways her eating disorder and low self-worth had kept her locked away from opportunities to explore her interests and engage more with others. I learned that she’d always wanted to take a pottery class, go on a road trip to some historical sites, and learn more about birds.
“Instead of waiting for the magical moment of readiness or perceived deservedness to do these things,” I said, “what if we figured out ways for you to do them now?” As is common for people living in larger bodies, Diane felt she couldn’t pursue these kinds of “normal life” things until she’d lost more weight, even though experiencing those things first is often exactly what’s needed to make progress with eating changes. At this point in our work, she greeted the prospect with vigor.
Diane also grew open to the idea of exercise but didn’t want to get sweaty in public or feel inferior at a gym; she’d already had way too many experiences of being ridiculed in those situations. “Let’s not even call it exercise if that makes you cringe,” I suggested. “How about we look for ways to find joy in moving?” She loved the idea of getting more creative about finding ways to engage in more movement while steering clear of fat-phobic places. She also eventually agreed to join a group for women with BED, which helped to decrease her sense of isolation and “being different.”

Diane has continued to lose weight, sometimes only a few pounds in a month, and to take steps toward normative, mindful eating, as well as positive activity routines. Recently, she took a vacation to one of her bucket-list locations, Rome. She was annoyed with having to ask for an extender seat belt on the airplane and with having to take frequent breaks while walking around the city, but she had much more to say about the sites she’d seen and the excitement of travel. She’s also started experimenting with recipes and cooking several times a week. “I don’t have to be embarrassed that I like to eat good food,” she tells me now, “and taking the time to make good, healthy food for myself is part of my self-care.” Our work is ongoing, but our sessions are less frequent now. Most importantly, she’s no longer just waiting for the weight to come off before making important changes toward physical and emotional well-being.
Case Commentary
By Lisa Ferentz
I appreciate Sandra Wartski’s depathologizing approach with Diane and her recognition that binge eating isn’t just about food. I also support her emphasis on nutritional education, helping Diane realize that dieting doesn’t work and restricting calories fuels subsequent bingeing. However, I believe Wartski is conflating two issues here—binge eating and morbid obesity—in a way that’s both ethically and medically problematic.
Although I understand the therapist’s shift in focus from “weight to wellness,” wellness is connected to weight in this case. There are serious medical complications to consider when someone weighs 350 pounds and has a BMI of 50 to 60. Diane’s weight has caused considerable suffering physically, emotionally, psychologically, and medically. Therefore, encouraging her to continue to explore with her doctor a risk/benefits analysis of surgery should be an ongoing component of treatment. After all, there’s a reason Diane’s doctor presented the option of surgery several times; he or she understands that Diane’s weight is life threatening, increasing her risk of developing and prematurely dying from a wide range of medical complications.
It seems that in a compassionate attempt to destigmatize Diane’s obesity, Wartski has minimized Diane’s life-threatening condition. If Diane were anorexic and weighed 70 pounds, would the therapist be content with her gaining only one or two pounds per month? In both cases, “weight maintenance” would be dangerous.
Additionally, Diane’s weight gain hasn’t been put in context. Why has she gained 200 pounds since college? It would help to further explore the metacommunication of her binge eating. Is she creating a protective shield around her body to keep people at bay? Is there a punitive component to her binge eating, and if so, why does she feel compelled to hurt her body? I certainly see that amount of weight gain as a form of self-injurious behavior. Similarly, it seems that the connection between Diane’s bingeing and childhood/adult trauma hasn’t been adequately processed or resolved, making the decrease in the frequency of sessions problematic.
When emotional eating is uncovered and understood, it’s important to offer clients alternative strategies for self-soothing and affect regulation to reduce inevitable relapses. I like the therapist’s focus on increasing self-compassion and decreasing shame, but I don’t think weight-loss surgery would negate behavioral and emotional strategies. For clients whose weight is life threatening, surgically achieving significant and lasting weight loss, combined with behavioral changes, reducing dissociative eating, creating a new relationship with food, and teaching alternative self-soothing strategies, is the best and most ethical way to address their physical, medical, and emotional well-being.
Author Response
I appreciate Lisa Ferentz’s commentary about this case, but would like to respond to a few points. Diane had spent too many years fixated on the numbers on her scale, and this ended up being counterproductive. Diane responded well to the broader notion of overall wellness and became committed to addressing her weight in this different, nonshaming way. Through collaborative contacts with her treatment team—her medical doctor, psychiatrist, group therapist, and nutritionist—we continue to focus on the fuller dimensions of wellness, not just her weight, while her physician carefully monitors her closely with regular lab tests and office visits.
Although Diane is still losing weight, periods of plateau and weight maintenance naturally occur, just as they often do for people in treatment for anorexia. She needed help understanding that the expectation of significantly dropping pounds at every single weigh-in is unrealistic, but the goal of decreasing her weight remains a focus for her. And when we notice plateaus, we always explore the details to make sure no new negative patterns are forming and that her behavior is still supporting the overarching goal of weight loss.
As Ferentz suggests, there are multiple, complex reasons for Diane’s binge eating, which we’ve continued to address in treatment. Space limitations didn’t allow me to write at length about the details of her history, various comorbid factors, and other aspects of this case that have emerged over time, but they are, of course, an important part of the work. For example, we’ve spent time processing past relationships with abusive boyfriends and how those experiences have shaped her relationship with her body. We’ve looked at how other traumas led to her further shutoff from the world, and how her larger body has indeed kept her from connecting with others for years. We’ve explored how food became a legal and cheaper substitute for the drugs she used in her early 20’s.
She has come to see how her overeating moved from being primarily a way to soothe and cope to being a more multifaceted way to comfort, numb, celebrate, punish, and pacify. This case highlights a wide range of issues with food commonly encountered in treatment, but I focused on the psychoeducational aspects of working with BED not often addressed in therapy.
Lisa Ferentz
Lisa Ferentz, LCSW-C, DAPA, is a recognized expert in the strengths-based, de-pathologized treatment of trauma and has been in private practice for more than 35 years. She presents workshops and keynote addresses nationally and internationally, and is a clinical consultant to practitioners and mental health agencies in the United States, Canada, the UK and Ireland. In 2009 she was voted the “Social Worker of Year” by the Maryland Society for Clinical Social Work. Lisa is the author of Treating Self-Destructive Behaviors in Trauma Survivors: A Clinician’s Guide, 2nd Edition (Routledge, 2014), Letting Go of Self-Destructive Behaviors: A Workbook of Hope and Healing (Routledge, 2014), and Finding Your Ruby Slippers: Transformative Life Lessons From the Therapist’s Couch (PESI, 2017).