We all have moments in life that create an irreversible chasm between what was and what will be. Mine happened when I was only 29 years old, on a warm day in June, the so-perfect-it’s-cliché time for weddings. The chapel is packed beyond standing room with people; they’ve overflowed into the parking lot. There are flowers all around me. Soft music plays as guests greet each other in a reverent hush.
All of this was meant for my wedding. Now it’s for a funeral instead.
The flowing fabric of the brightly flowered sundress I’m wearing feels out of place. My usual streamlined black attire would have been more appropriate. But this was supposed to be my day to wear the white gown while celebrating life and love. With this in mind, I’d forbidden black at the funeral. Johnny was about light and joy, and I’m determined that today we will celebrate his life despite the despair that threatens to engulf us.
I’m raw, gutted, my chest so tight I can barely breathe. Between the people who pass by to express their sympathy and personal sadness at the loss of this beloved man, I flash out of black despair into indignation and rage. I’m a bride! Where’s my joy? My forever?
I shakily ascend the steps of the church’s lectern stage and open my old leather journal to begin my eulogy. I barely hear the words coming out of my mouth over the question spinning through my head: How am I going to get through this? A notion—maybe a prayer—rises in my mind, that halfway through reading these words, the same thing that took Johnny from all of us might also take me. I’ll collapse on the floor in a heap, my lungs failing to take in air—respiratory failure. My heart failing to beat—cardiac arrest. In dark agony, my mind pleads with the universe. Please! There has to be meaning in this.
As a clinical psychologist who’d specialized in the neuroscience of traumatic stress, I thought I understood trauma. However, after my fiancé’s sudden death, my mind is overtaken by grief, plunging me into a relentless agony so dizzying that it takes me a few months to recognize I need trauma-informed care—which is to say, sensitively administered treatment with a therapist who can understand the nuances of traumatic grief, hold space for my vulnerability and raw pain, and help me heal toward a new future.
Finally, I reach out to a grief therapist I’ve been referred to. Sitting nervously in her waiting area, I watch the minutes tick past on a clock. My new therapist doesn’t emerge from her office to call my name until 15 minutes into my session time. As she invites me in and motions for me to sit on the sofa, she inquires, “So, what brings you in today?”
I know my face registers shock. I’d spoken to her on the phone just two days ago, giving her details that would tend to be memorable to most people: finding my fiancé dead one week prior to our wedding and not being able to resuscitate him, the wedding turned funeral, the referral from her colleague across the hall. But she doesn’t seem to remember.
Starting to feel queasy, I relay those details again, watching her face for some glimmer of recognition. Finally, something seems to jog her memory. She gives me a soft smile that helps me relax a tiny bit.
That doesn’t last long.
“Oh yes,” she says, “you’re the widow.”
Until that point, I hadn’t thought about that term—or any label for my new relationship status. Widow—is that what I am? Is that the label for when your soul feels dead, and you’re fighting to keep what remains of you alive?
This pivotal early interaction with a therapist should’ve been marked by a sense of safety that could help prop me up during the most difficult time of my life. But the startling forgetfulness, followed by the nonchalance with which she wielded the term widow, was deeply unsettling.
Trauma-informed care means receiving a person’s story in its entirety, acknowledging the unique context, and fostering a therapeutic alliance based on psychological safety, compassion, and respect. It means not reducing someone’s acute and fresh traumatic event to a label. Crash victim? Rape survivor? Former homeowner and fire escapee? These lock our clients into a narrow role they never asked to play.
Not taking the needed steps to create a healing space that affirms the client’s humanity risks retraumatizing the people in our care. For me, the result was the onset of PTSD, which would plague me for five years.
“So what happened?” the therapist asks next.
I pause, not understanding the question. Does she want to hear about the 10 years of love we shared? Or how our wedding had turned into his funeral? I must’ve paused too long because she redirects me with another question.
“Sometimes people find it helpful to start at the beginning of the day their partner died. Please feel free to start there. Or tell me about the moment you found out he was dead.”
A small part of me is grateful for some instruction, but the rest of me is horrified. I’d only told the full story of that night to the EMTs, the police, and the coroner. In fact, I can barely remember anything that happened after I’d come home from being out with my girlfriends, found John on the floor, and grabbed the phone to make the 911 call. And I want to keep it that way.
As the silence in the room lengthens, I can tell she’s starting to feel uncomfortable. That’s not helping my own uneasiness, or my people-pleasing tendency. Discussing the pain is what you’re supposed to do in therapy, I remind myself. I mean, she’s the grief specialist.
At this point, my brain feels foggy and my head heavy, as if a soothing steel blanket is wrapping around me to shield me from the pain. I recognize this for what it is—I’m starting to dissociate.
As she looks at me expectantly, I have a mental image of reaching into my skull and clawing apart the steel blanket so I can access my emotions. But the metal cocoon just keeps snapping back into place, cutting me off from the pain and blocking my ability to feel or even remember.
Finally, in a robotic voice, I walk her through the final hours of John’s life as I know them. Blunt data points pile up on the carpeted floor between us until, when I try to provide an ending to that awful night, my brain greets me with a yawning blackness. It seems I have no idea what happened after they took John’s body away that night and I was driven to a friend’s house. (To this day, I still don’t.)
In response to my story, she quirks a single brow at me and delivers that famous therapist line: “And how did that make you feel?”
How did that make me feel?!?
It’s all too much and my numbness gives way to an avalanche of agony. I feel a lifetime of loss and pain crashing down on me, and I curl in on myself, becoming a tiny ball on her sofa, forehead on my knees. I just want to die, I think, but I have the presence of mind to know that I can’t trust her with that statement. Instead, I shake my head and take some shuddering breaths.
The minutes thunder severely in the silence as I attempt to ground myself back into my body. When I finally look up, I catch her staring at the clock. “Unfortunately, Kate, that’s all the time we have for today,” she says.
I’m shocked, shaking; I can’t gather my focus enough to say anything. Meanwhile, the therapist pulls out her paper calendar, clearly punctuating the end of our session, then says, “I have the same time available next week—does that work for you?”
When I don’t answer she looks up, and finally seems to register that I’m really not doing too well. She flips her calendar back a page. “Perhaps sooner would be better? I can fit you in this Thursday at 2 p.m.”
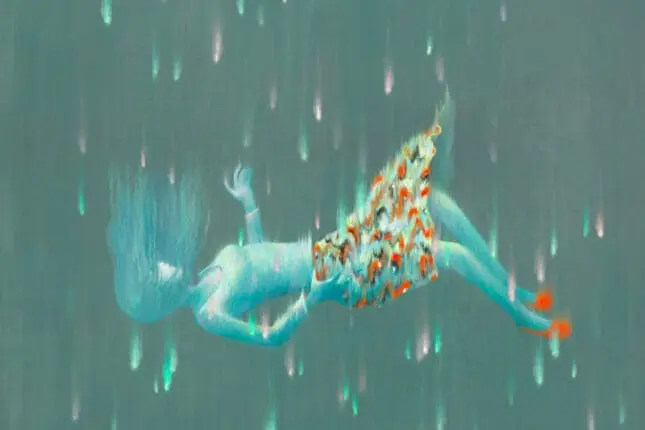
I nod woodenly, desperately grasping for my steel blanket of dissociation, but I can’t quite pull it up over my head. There’s a sensation that the floor has dropped out from underneath me and I’m falling.
“Yes, Thursday at 2:00 p.m.,” I murmur. I take the appointment card she hands me, gather my things, and exit the office into the bustling foyer. Only when I encounter the receptionist’s look of alarm do I realize that I’m weeping.
Needless to say, what I experienced that day was not trauma-informed care. I didn’t have the grounding presence of a therapist who was armed with an understanding of the need to resource and cultivate psychological safety prior to asking a client to recount a traumatic experience, especially a recent one. She didn’t proceed gently or thoughtfully with me. When I got home, my brain began to loop in a Technicolor version of that awful night John died. I revisited each moment in agonizing clarity, dissecting my choices, and going to some very dark places.
Now, I know that how that therapist posed the question of what had happened that night, and when she’d posed it, could’ve made the difference between grounding me versus sending me into an emotional freefall. But in the wake of that therapy session, my protective friend, dissociation, disappeared. What little sleep I got was disrupted by nightmares. And in my waking hours, I even spiraled into hypnagogic phenomena—where the brain produces vivid visuals that in my case were horrific and accompanied by a traumatic sense of loss. Sometimes, as my brain tried to make sense of the nonsensical, I even experienced a felt sense of John in the room.
On Thursday at 2 p.m., I walk back into that busy foyer and sit in the same chair. When I say I have an appointment with the therapist I’d seen before, the receptionist shakes her head at me and replies, “She’s not here.”
“Excuse me?” A gnawing anxiety rises in my gut. “What do you mean?” I’d built up a story in my head that even though the first session had been terrible, and the following three days even worse, this one would bring me back to some semblance of balance. My voice climbs a couple octaves as I say, “Please call her. We have an appointment.”
“I’m sure you got the date and time wrong. Weren’t you just here?” she responds.
Is this really happening? Did I get the date and time wrong? No, she wrote it down. There’s no way I had it wrong, right? I start to shake. Tears threaten to fall. This is awful. I’m losing control. What’s wrong with me?! I can hear my thinking brain judging me, priming me for a shame spiral of epic proportions, while my survival brain screams, I need this session. I’m scared. I need help.
My voice, edged with panic, strangles out a pitiful request. “Please call her.”
I can tell the receptionist is getting nervous. She doesn’t move. Desperate, I fish around in my purse until the sharp point of the appointment card pricks my fingers. I brandish it at her. “See?”
Assessing the card, she begrudgingly picks up the phone. “I have a patient of yours here. She says you have an appointment. Her name is . . .” She looks at me inquiringly.
“Kate,” I mouth at her.
“Uh, Kate.”
I hear the therapist on the other end of the line. “Oh, shoot. I completely forgot about her. Let her know we can reschedule for next week. I need to go.”
The receptionist hangs up and gives me a pitying look. “Would you like to reschedule?” she asks.
I shake my head. Absolutely not. Internally, I’m still grappling for that steel blanket of dissociative numbness. It remains stubbornly absent. I don’t know what I’m going to do.
When people hear about this false start—setback, in fact—to my healing, they’re outraged: I’ve received texts and phone calls from many colleagues expressing their anger. Their reaction feels validating, but it’s not why I’ve shared this story. I do it as a reminder that as therapists, we’re human, we’re fallible—and while what happened to me in therapy may seem like a major violation, it’s a common one. If we’re honest, all of us have probably had moments in which we’ve accidentally stepped into a similar mess with clients.
My desire isn’t to blame this therapist for her poor treatment of me. My goal is to shine a light on the need for trauma-informed care—not just as a buzzword we attach to our professional bios, but as something practical that can save a real client from real, preventable emotional damage. In my case, that damage included flashbacks, nightmares, and suicidal considerations. But there was a silver lining: eventually, I found an alternative, holistic way of approaching my own care that also changed the way I practice psychotherapy: a psychosensory approach similar to EMDR and Tapping that aligned with my neuroscience-based training. Had I not journeyed through the darkest corners of trauma—including trauma exacerbated by negligent, misattuned care—I wouldn’t know in my bones what it takes to heal.
***
Adapted with permission from Keep Breathing. Copyright © 2024 Kate Truitt, Keep Breathing. All rights reserved.
ILLUSTRATION © JORM SANGSORN
Kate Truitt
Kate Truitt, PhD, is a clinical psychologist and applied neuroscientist. She’s the founder of the Truitt Institute, an educational platform dedicated to advancing access to mental health support on a global level, and she leads the award-winning clinical group Dr. Kate Truitt & Associates. She’s a developer and chief science advisor of the Havening Techniques, and the author of Keep Breathing and the international bestseller Healing in Your Hands.