Twenty-year-old Lara is sitting where she always sits, as am I. She’s comfortable here and surely knows how much I enjoy her. She has a new relationship and a new tattoo. Her dad knows about the former but not the latter. “He’d kill me,” she says. “After my first tattoo, he told me he wouldn’t help me pay for classes if I got another one.”
“Well then, you’re playing with fire,” I say.
“He won’t follow through. I can hide it from him anyway. And ohmygod I’m 20. It’s my body!”
Lara and I have spent many sessions dealing with her loving but anxious, overprotective father. And because I’ve known her since she was 12, her father was present for most of those sessions. I specialize in anxious children and teens, but I don’t see them alone. Anxiety is a family thing, and parents need coaching. Generational patterns aren’t broken by 10-year-olds sent back into an entrenched dynamic, armed with breathing exercises and reassurance. The rule in my practice: if you can drive to your appointment alone, you can come to your appointment alone.
Although we still have occasional family meetings, Lara now comes in on her own. We’re on the upside of a serious crisis that happened when she went away to college, almost two years ago. Given how capably she was managing her anxiety, I didn’t actually see her much during her junior year of high school and not at all her senior year. But after her first year in college, she was depressed, failing academically, cutting herself with razor blades, and filled with shame. Once home, she came straight to my office.
Lately, I’ve become aware of just how much of my practice is made up of young adults like Lara, whom I’ve known since they were little. In part, this is the natural result of having lived and practiced in the same town for almost 20 years: my teacher friends now have classes filled with their former students’ children; last week, I saw my son’s former babysitter pushing her baby in a stroller. But this pattern is also indicative of a generation of young people in trouble, stuck in the transition between childhood and adulthood. Unable to let go of one trapeze and trust that another is heading their way, they feel more scared and alone than ever.
Jane Brody, in her New York Times article “A Road Map Out of Loneliness,” writes of the high incidence of loneliness and isolation in 18- to 24-year-olds these days, and its unsurprising correlation to suicide. She adds that loneliness in this age group is far higher than in the elderly—as much as 50 percent! Jean Twenge’s recent article in The Atlantic, “Have Smartphones Destroyed a Generation?” describes teens spending less time with friends and feeling less connected to parents, despite spending more and more time under the same roof with them.
So what’s my role with my “long-term” clients in this age group who leave the nest for college but keep swinging back for therapy? Sometimes I wonder if there’s something contradictory about my practice. I describe myself as a brief therapist, who from the first session works to identify the therapeutic target and teach skills to address it. I bemoan unnecessarily prolonged multisession assessments and am adamant about offering parents and children concrete instruction immediately. Yet I’m starting to revel in the decades-long connections I have with certain clients, in the privilege of being there as they wade through the tween years, navigate adolescence, and venture into adulthood. I’ve come to realize that I can simultaneously be an important connection in the present, right here, and a conduit to the real world, out there.
Treatment with these clients usually begins when parents recognize that anxiety has taken over parts of their child’s life: school attendance is dropping, isolation or explosive behavior is increasing, or physical symptoms are dramatic. After they learn as a family how to recognize and manage the worry, long remissions are common. I rarely see them every week, or even every month. Rather, over the course of the years I know them, these families show up at predictable milestones, like the start of middle school or high school.
Some think preventively, returning to therapy in preparation for a transition. Others call when a crisis occurs and the anxiety grabs hold again: a divorce, the discovery of substance abuse, a broken heart, a diagnosed illness. With clients like Lara, the launch from home doesn’t go as planned. They return feeling lost, and tears come easily, but we’re always happy to see each other.
Swinging Back
Lara and her parents first came to see me when she was in sixth grade. She was a spectacular student, had just played the lead in a community theater musical, and was friendly and popular. The issue, her mother told me, was a recent series of “panicky freakouts” when Lara was sleeping at friends’ houses. “I think about what could happen, and I start feeling sick,” Lara told me. “Then I call my mom and go home.”
Although sleepover trouble was the presenting problem, Lara was a typical worrier, with an imagination that would “what-if” her into panic. She followed the predictable process of anxious children and adults: when faced with an uncertain situation, she anticipated what might happen, imagined how awful it would be, got a tummy ache, and then escaped the situation to feel relief. Understandably, she began to avoid anything tinged with uncertainty, choosing to stay home more and more so as not to trigger anxiety. She was, in effect, worrying about worrying, and avoidance became her best strategy. But because Lara was so high achieving, even at such a young age, the avoidance that worked for her in the short term left her angry and disappointed with herself in the long term.
Lara, her parents, and I went right to work. The content of Lara’s worry, they learned, was not the issue. Instead, their task was to become familiar with the process of her worry—how it showed up and demanded certainty—so they could learn how to respond differently to it. Avoiding uncertainty, they came to understand, only made the process more entrenched. So they began to purposely confront uncertain situations as a family, recognizing and talking back to the worry that ensued. Lara’s father even began to see how his own anxiety had always held the reins, and what this modeled for everyone else. As he was increasingly able to take an active stance in demanding the reins back, Lara too got better at maintaining an offensive position with her worry.
I continued to see them during Lara’s first two years of high school, often meeting with Lara by herself for a portion of the session. During this time, she revealed she was having intrusive thoughts, strange and disturbing worries that she’d do things she had no intention of doing, like telling a lie to her teachers for no reason, or stealing something from Target when shopping with her mother. “But what if I did?” she’d ask me repeatedly.
Again, our work together focused on how to step back and identify these thoughts for what they were: annoying but irrelevant. She learned about her OCD patterns (and her father learned about his), and by her junior year she became a whiz at allowing the thoughts, however bizarre, just to be there and be meaningless. Interpretation or analysis only made the pattern stronger, creating what therapists Martin Seif and Sally Winston call entanglement, the process of “fashioning meanings and warning signals out of passing mental detritus.”
At one point, Lara was pulled into a thought that she might’ve cheated on her sophomore biology final. The pattern was predictable. “I know I didn’t cheat,” she told me, “but I kept thinking I might have without realizing it.” She’d asked her parents about it several times the day after the exam, but they recognized the thoughts for what they were and told Lara so. She was able to move on quickly and even with some humor, a victory for sure.
Lara’s parents sent me a sweet note when she graduated, letting me know she was headed off to college. I texted her to wish her luck. She texted back that she planned to major in business and was excited to be away from her parents.
The next time I saw her, she was in my waiting room. The first semester had gone well, but she’d barely gotten through the second. She’d told no one she was struggling, skipping classes, ignoring professors when they’d reach out. She’d spend time with friends and this perhaps sustained her, but she couldn’t shake her increasing sense of panic and hopelessness. She didn’t want to go back.
Her parents learned of her state in dribs and drabs. She’d failed several classes. She was on academic probation. She was having panic attacks. She was depressed and had some suicidal thoughts during the worst of it. They came for family sessions, but she, as a legal adult, controlled what they knew and didn’t. The parent–child relationship was moving into a new stage, and roles were changing fast, including mine.
It’s common for symptoms to reemerge when life gets more complicated or changes course, so I honestly wasn’t surprised to see her. My job is often to revisit what my clients already know and then talk directly about the prevention in the future. I knew she had the strategies—we just needed to bolster them up, reactivate them. We talked about what she ignored or lost track of in herself, and asked important questions that this young adult needed to address: how will she know in the future to seek help? How and to whom will she communicate her feelings of being overwhelmed when they arrive? What are the signs she must recognize when she’s on her own?
Had I been meeting this distraught family for the first time, I can imagine being a bit overwhelmed with all that was happening. Most clinicians know exactly what it’s like to sit in those initial sessions with a person in crisis, when you hope you’re making the right moves, feeling both responsible for what happens and a newcomer to the party. But here’s where the years of connection made all the difference with Lara and her parents. In the midst of this crisis, I didn’t need to sort through their history, their relationships, their coping strategies. Like the small-town family doctor, I had access—not always the case with a young adult—to the bigger, fuller family portrait.
Perhaps most valuable during this tough phase was the trust that already existed among us all. Because of our connection, Lara’s parents trusted me enough to be direct, to ask me pointed questions, and to tolerate the discomfort of what we were discussing together. And I trusted them as parents. I’d seen their ability to follow through, to be loving and open, and to recognize when their own anxiety was perpetuating Lara’s or getting in the way of treatment.
Lara trusted that I could help her and, given her previous experience with my approach, knew I’d require her to do things that might be uncomfortable: communicating with her roommates at school about her plans to take a year off, returning to her part-time job at home, and exercising at least three times a week. She was self-conscious about being back home, and not sure how to respond to the normal questions people would ask her about her first year at college. Her anxiety magnified her fear of how others would react, the uncertainty of what they’d think about her. We knew her anxiety and depression would fully support avoidance, so she needed to do the opposite: step in, communicate, get out of the house, be active.
Our past success together created a positive expectancy that made the process move more smoothly. We could talk openly about the cutting she was doing at school and how she could share her thoughts, concerns, and feelings with her parents without such discussions turning into conflict and fueling feelings of isolation. We framed her panic, depression, and withdrawal during her second semester as a “bad breakup with her future plans”—she’d gone off to college certain of her career path (and with her parents’ enthusiastic endorsement), only to discover it wasn’t what she wanted.
She’s now spent this past year at home recovering from this breakup, being unsure of how the rest of her life will go, taking classes at the community college in town, and exploring what’s next. Her energy has returned, and she’s discovered a new career interest, quite by accident: working with an organization that trains service dogs. I’ve tracked a wonderfully normal push-pull with her parents as she’s bemoaned her father’s demand for a curfew and an equally normal sense of anxiety as she’s moved into a new intimate relationship and planned an adventure trip to Mexico with an old friend.
As we note each positive step forward, much of our time is spent talking about maintenance and prevention. In particular, we’re building a new pattern of seeking support and connection when the inevitable bumps of increasing autonomy and adult decisions leave her feeling unsure or even panicky.
Time for Adult Insight
Not every young adult goes away and returns in crisis. Often they come back for a bit of a booster, or a place to hash out their confusions about themselves and their life’s direction. This was the case with Jenna, who emailed me well in advance to schedule a session during a two-week visit home. At 22, she’s been living independently for a few years, taking college classes, and working to support herself.
I began seeing Jenna in middle school. Her mother was concerned that she was “boy crazy,” didn’t have solid friendships, and always seemed anxious and angry. They fought often. Jenna has a sister with special needs, which creates added stress in the family. In all the years I’ve known Jenna, I’ve never met her father, who works long hours and seems content to stay out of the fray.
Soon into my relationship with Jenna, however, her mother’s catastrophic parenting pattern became clear. Before our family sessions, I’d often receive an email from her describing the latest crisis and concern. Each time, nothing had happened yet, but, according to her mother, Jenna was on the precipice of something we needed to talk to her about. I once received an unexpected call from a relative wanting to let me know that nothing I was doing was helping, and that perhaps I wasn’t aware of just how awful Jenna’s behavior was.
Jenna could certainly be reckless at times. Some serious conflicts with friends flared up in high school, fueled by accusations of stolen boyfriends and texts that, Jenna admitted in time, had crossed a line. She also maintained good grades, started her own gourmet cookie business, and worked 20 hours a week in a retail store. She graduated with honors and made her own arrangements for a job and financial aid in a college out of state. Despite her seeming independence, I know how her crisis-based upbringing has left its mark. She often talks about herself in terms of her “diagnoses,” and leans toward the catastrophic when assessing her own health.
She arrives at my office, her hair a different color—purple—and with a few new piercings since we last met, about nine months ago.
“Am I late? I’m sorry. I just came from my doctor. She gave me another medication for my depression.”
“Your depression?” I ask, prompting her for details.
“Ugh, the last week has sucked. I don’t even want to get out of bed. I’m so grumpy, and I feel like I’m going to cry all day. I told my doctor, so she wants me to try Wellbutrin before my depression gets worse.”
Years of connection with Jenna and her family have taught me that her behavior and accomplishments are far more indicative of her functioning than the variety of labels and diagnoses she and her mother have embraced over the years, so rather than asking about her depression and the current medication, I ask her to fill me in on life. What’s she been doing? How’s school? Is she still painting?
“It’s been nuts!” she says. “Hasn’t it been nuts?” She then goes on to describe the busy life of a 22-year-old woman on a #MeToo mission. Now a political science and gender studies major, she’s started volunteering at a women’s resource center, advocating, marching, and doing grunt work on campaigns. She’s made great friends and has a new boyfriend, but she’s let her painting slip, because, with school and work and volunteering, who has time?
“How has your visit at home been?” I ask.
“My mother freaked out,” she says. “She told me that she doesn’t like all this ‘feminist’ stuff and that I’m turning into a different person. The hair was not a hit.” Her grandmother thinks she’s not “normal.”
Once again, I’m grateful for the years of history with Jenna and the benefit of a complete backstory. The women in her family have consistently seen her as a disaster in the making. Her mom once filled out the Vanderbilt ADHD Diagnostic Scales on her own in an effort to convince me and the school that Jenna’s energy, as her grandmother still fears, was a sure sign of trouble.
Jenna, I decide, is ready for a session designed to give her adult insight into longstanding family patterns. Because she’s been on her own and doing well for quite some time, the contrast between how she functions on her own and what happens to her mood within days of returning home is stark. I want to update the connection between what she’s observed in her family and her current reactions. And honestly, I want her to question the quick “diagnosis” that her depression is worse and another medication is needed.
My time with her is short, so I dive in, peppering her with questions. Can she begin to view herself—with all her strengths, weaknesses, challenges, energy, values—separately from her family’s view of her? Is being different from them a diagnosis? What’s her normal? How does she establish her own identity and remain connected to the family that she loves? How does she know when and where to seek out support?
I point out directly the correlation between her return home and her worsening mood and energy. I ask her what she imagined her interactions with her parents would be like. She tells me she wants them to be proud of her independence, and she wants her mother to stop freaking out.
“Sometimes you go into a Chinese restaurant looking for lasagna,” I tell her. “And you’re disappointed they don’t have lasagna.”
She wants lasagna, she tells me, pouting.
“You know you can go other places for lasagna. You’ve always done that, actually.” We talk about what her family does offer her, the positive things both her parents have taught her: loyalty, a good work ethic, responsibility, good money management.
Selfishly, I’ll admit, these sessions are a treat. I can explore a broader family perspective with young adults, something they weren’t as capable of as children. And I can talk realistically about how they have and will continue to update their support networks, relationships, and views of themselves.
Jenna leaves this session, like Lara, with a new frame to try out. Because she was raised in an anxious, catastrophic family, she has to choose what she’ll take with her and what she’ll leave behind. She can connect with them in different ways, not only through crisis and “illness.” I hope I’ve planted the seeds to the question I want her to continue to ponder: must you remain loyal to this family legacy, or will you allow yourself to grow out of it?
No Perfect World
In a perfect world, these long-term therapeutic relationships result in young adults who can solve problems, create positive relationships, and move through the ups and downs of plans getting interrupted and needing to be adjusted. But these relationships present challenges, too. Cooperative 11-year-olds become mutinous teens, tired of their anxiety, their parents, and me. After years of sessions, they decide I have nothing new to offer, and sometimes they’re right. Or they discover that alcohol and pot are more immediate solutions to their anxiety, disinhibiting them enough to be social or disconnecting them enough to not care anymore.
When they turn 18, those with anxious or overinvolved parents sometimes assert themselves by rejecting all support, despite my efforts to help them individuate in a balanced way. Or they may continue to see me, but shut down family members’ participation. While I see the appeal and advantage of this for some young adults, as a systems-focused social worker, I make my preference clear that they don’t cut out their parents. This adds a layer of complexity to my work with them and requires some boundary renegotiations, as I remain empathic to the frustration and helplessness the parents must feel.
Damon, for example, saw me for several years, starting when he was 15, for help managing his OCD. His mother was a worried and reactive parent, and his explosive reactions to his OCD resulted in confrontations between them, and subsequent phone calls from her requesting crisis appointments with me. I never made much progress in changing the dynamic between them. Damon blamed his mother’s genes for his disorder and had little compassion for her own struggles. He disappeared from treatment for several months at time, drank too much as a teenager, and put holes in the walls at home.
He eagerly awaited his 18th birthday, clear that he was now in charge of what he would and wouldn’t do to treat his disorder. Periodically, he’d rescind permission for me to communicate with his mother, and then change his mind. His mother continued her attempts to get him into various inpatient programs, requesting that I fill out provider referrals. But he easily sabotaged admission by describing himself during the intake interviews as violent, noncompliant, and uninterested.
Damon is now 23. The last few years have been bumpy. He moved out of state for almost a year, but came back home after a series of disappointing jobs and relationships left him depressed and broke. The conflict between him and his mother resumed immediately. He came for sessions sporadically, often arriving fresh off an argument at home. I last saw him several months ago, when he told me he was done with therapy.
As I look back over the years, I wish I could’ve helped untangle the family conflict. I couldn’t find a way for either Damon or his mother to recognize what they had in common and work together on their shared “curse,” as Damon called it. Perhaps he’ll return as he has in the past. Our relationship, I believe, will make it easier for him to come back when he’s ready.
How Did We Get Here?
As I write this, several of the young adults I’ve known for years are moving to the edge of the nest, preparing to leap. This affords me the opportunity to review our years together. I want to take stock of the steps we’ve taken and the ones we’re putting in place to support a successful launch. One fledgling, Liza, came for a session with her mom just last week.
From the moment she sat down, she was bubbling with anticipation about her upcoming move away from home at the start of the semester. I asked them both, “How did we get here from where we started?” It was a long way from when an intensely anxious Liza had been 12 and already ruminating about the eighth-grade camping trip more than a year away.
At that time, for as long as they could remember, her mom, Dana, had sat by her bed every night until Liza fell asleep; and over the course of the day, she’d diligently try to help Liza avoid anything that felt “weird” or might involve “weird people.” Once, Dana and her husband had tried to have a weekend away, but Liza was so distraught the entire time that no one had fun, including the sleep-deprived grandparents left in charge.
I opened Liza’s folder and begin reading my progress notes aloud to both of them. It turned out we’d forgotten many events, like the time she’d vomited at cheerleading, or the way she’d handled a teasing episode in Spanish class. We were surprised, in retrospect, how quickly the sleep issue resolved, even though the three of us agree it had felt at the time like it dragged on forever.
I didn’t share my notes on a session I’d had with Dana alone, days after the school shooting in Newtown. She’d arrived for our planned session without Liza, needing to talk about what had happened. How, she’d sobbed, can she allow her children more independence in the world when this is a reality? How can she leave them alone in their beds with those horrific images in her mind? We’d sat together as two moms, wondering the same things, stepping both toward and away from the unspeakable pain of the Newtown parents.
That day, Dana had also shared more about her own anxiety and how it affects her parenting. I’d already known she was an anxious mom, and she had, too. But she’d told me details about the trauma of her own mother leaving the family and how abandoned she’d felt as a young girl. Like many anxious parents who’ve experienced profound separation from a parent, she wanted to protect her own children from any such pain and protect herself from any more loss. We began the first of many conversations about how to differentiate herself as a parent from the abandonment she’d felt as a child, and how to cultivate a loving connection with Liza—one that would support her daughter’s budding autonomy.
Anxious parents tend to convey that the world is a dangerous place, and their overprotection inadvertently sends a “you can’t handle this!” message to a child. Over the years, together Liza and Dana had learned the patterns of worry, and how stepping into uncertainty and discomfort are a normal part of growing and maturing. Little by little, they’d experienced the difference between crisis worry and normal worry. Liza had been allowed to solve problems on her own, and Dana had pulled back her constant reassurance.
So when I asked them both how we’d gotten to this point, Dana laughed. “I owned my shit,” she said. “I did what you told me to do.” She meant that she’d followed the plans we’d created in therapy, let Liza fall asleep on her own, stopped texting her during school, promoted sleepovers, and gone on an out-of-state trip without her daughter. When I told her last year to delete the app that allowed her to track Liza’s every move, she did, that night.
Liza deserves kudos for her hard work. She’s heading off with such eagerness and flexibility because she, too, was an active participant. As I take stock of her growth, I’m most pleased with her willingness to look at her own patterns and then to take a risk by doing the opposite of what her worry predictably demands. When she’d first thought about that eighth-grade camping trip, she’d been terrified of not falling asleep. By the time she’d headed off on the trip, a year later, her plan—just to foil her worry’s demands—was to stay up all night. (She fell asleep in the tent with her friends, of course, after a full day of hiking.)
She now almost reflexively resists her anxiety’s demand for avoidance and certainty. She moved through the roommate selection process aware that even the best matches can flop. “We’ll see how it goes,” she says. (In case you haven’t experienced picking a college roommate in the social media era, it’s become a combination of Match.com and being chosen for kickball in fourth-grade gym class.)
How will Liza fare when she heads off on her own? I’m optimistic. Unlike the parent blaming that keeps Damon spinning, Liza has learned—remarkably between the ages of 12 and 18—to take responsibility for her own patterns and address them with little defensiveness. Session after session, I’d point out how her decision to skip a school event probably hadn’t been because the other girls were mean, or she’d had a stomachache, but because her anxiety had been calling the shots. Eventually, her stance changed from “Who cares? It’s stupid anyway!” to a more insightful and honest “My worry is telling me not to go, but I want to, so I’m going anyway.”
Her openness to new experiences has grown over the years as her mother modeled this for her. We’ve prepared for the inevitability of conflicts and challenges. Dana knows how to let Liza struggle a bit, and now understands the difference between supporting and rescuing.
Oh, and we scheduled a session for Liza in December when she comes home after her first semester of college. We’re not done. All three of us want a check-in, perhaps a postgame analysis of her challenges during the first semester, or a happy bragging session full of her many successes. The appointment after her fun-filled camping trip, Liza and Dana arrived with cupcakes—we’re good at celebrating.
As a therapist, I don’t aim to be the main source of deep connection for these young adults. Quite the opposite. But my role as therapist is undeniable. Sometimes, at critical moments, I’m the lifeline, the hope, the constant. Sometimes, I get to be the cheerleader, the reality checker, the teacher who both models the new possibility and guides the skill-building that results in solid decisions and healthy relationships.
Therapy ends for all sorts of reasons. Plenty of families see me briefly. I often do one-time consultations. People get what they need and move on. But it seems that these young clients making the transition toward adulthood may be in more need than ever for ongoing connection and an open invitation to return as needed.
Is it the best strategy? Will it backfire? If we can use the connection to teach skills and normalize the uncertainty of transition, then I don’t believe so. Sometimes it feels like a replay of what toddlers do on the playground: venturing out and running back, just to check in, hand us a little treasure, receive a little encouragement, and then head out again. Twenty-nine years into my career as a therapist, as I witness these young adults move into the world, this type of connection and continuity feels more vital than ever.
Want to earn CE hours for reading this? Take the Networker CE Quiz.
PHOTO © SVETIKD
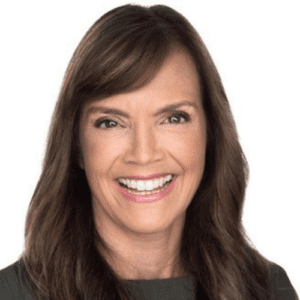
Lynn Lyons
Lynn Lyons, LICSW, is a speaker, trainer, and practicing clinician specializing in the treatment of anxious families. She’s the coauthor of Anxious Kids, Anxious Parents and is the cohost of the podcast Flusterclux. Her latest book for adults is The Anxiety Audit.