Enjoy the audio preview version of this article—perfect for listening on the go.
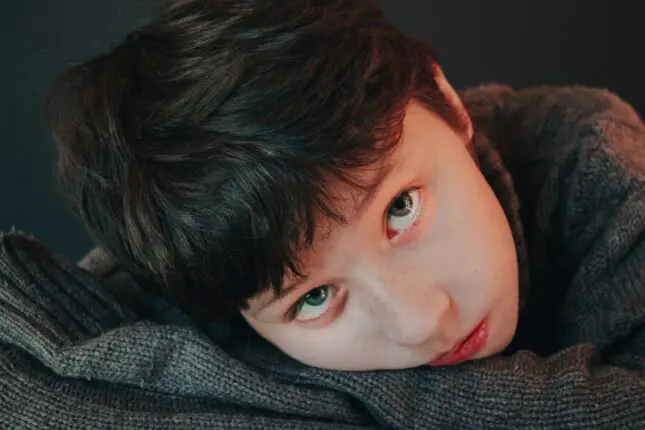
When it comes to treating children with ADHD, here’s the pattern I’ve started seeing everywhere—in therapy offices, homes, and schools. Once a week, therapists spend 50 minutes teaching a child how to regulate emotions, helping them learn to problem-solve, supporting them in honing social skills—and then, at the end of those 50 minutes, they send them back into a family system, school, and community that hasn’t been taught the same language or lens. In essence, we’ve been asking ADHD children to carry an impossible burden. We’ve been expecting them to change not just themselves, but the world around them. No wonder everyone—children, parents, teachers, therapists—feels stuck!
We’re trying to fix the child while leaving the environment exactly the same. And for kids with ADHD and executive function challenges, that almost never works. Here’s what I mean.
When I train therapists who work with kids with ADHD, I hear the same story again and again. It usually comes out halfway through the day, once we’ve settled into real talk. “The sessions go great… but nothing changes at home.” Heads nod around the room. They describe doing good, thoughtful therapy—the kind of therapy we’re trained to value. They’re helping kids name feelings, build coping skills, practice self-reflection. The child is engaged, insightful. Trying. And then the parent shows up the next week and says, “We’re still fighting every night about homework,” or, “Mornings are still a disaster,” or, “Nothing we talked about seems to stick.” Frustrating, right?
And then comes the perennial question: “What am I missing?”
Therapists who don’t have an answer often start reaching for more strategies. More consistency. Better follow-through. Clearer consequences. But the real issue isn’t the work being done with the child. It’s that we try to change the child while leaving the environment exactly the same.
Why Pull-Out Work Isn’t Enough
A few years ago, when I was leading a therapist training, I found myself thinking about how schools handle speech therapy. Usually, a child gets pulled out of one of their classes for an hour each week to work with a speech-language pathologist. The clinician does excellent, specialized work. The child practices sounds, learns strategies, makes progress.
And then they walk back into a classroom where no one else knows what they just worked on.
The teacher doesn’t reinforce it. The parents don’t know what to practice. The child is expected to somehow generalize the skills they’ve learned alone.
We would never expect that to work. Yet this is often exactly how we approach therapy with kids with ADHD.
Before going further, let me be clear: This is not about blaming parents. The parents I meet aren’t resistant. They’re exhausted. They come to see me believing their child “isn’t listening,” “doesn’t care,” or “knows better but won’t do it.” They’ve tried sticker charts, consequences, withdrawing privileges, and heartfelt talks. Some feel guilty. Some feel angry. Most feel both.
What’s usually missing isn’t another intervention. It’s perspective.
We think we understand ADHD because we recognize the headline symptoms: attention, impulsivity, and hyperactivity. But what I see, over and over, are skill gaps that live underneath those labels. Executive function challenges that shape everything about a child’s day—how they start tasks, hold information in mind, shift gears, regulate emotions, recover from mistakes. These aren’t matters of willpower. They’re developmental skills. And skills can’t be expected to show up before they’re built. I often explain this to parents by walking them through one specific skill: working memory.
There are different kinds of memory. Short-term memory is remembering you need milk, eggs, and juice. Long-term memory is remembering your childhood phone number. But working memory is the ability to hold and use information in the moment. It’s what allows you to follow multi-step directions, plan, and keep track of what you’re doing. It’s often described as the brain’s search engine, because it allows us to hold information in mind while we use it. When its weak, information slips away quickly.
So, when a parent says, “Go upstairs, get your backpack, your shoes, your tennis racket, and on the way down grab my water bottle and turn off the light,” they’re expecting a child to access working memory. But what if the child hasn’t fully developed that skill, yet? When they come back downstairs with one shoe on and nothing else, it looks like defiance or laziness. Parents feel frustrated, hopeless, and even angry.
But many kids with ADHD have weaker working memory. And this has nothing to do with their intelligence level. In fact, a large population of people with ADHD fall into the “twice exceptional” category: very high IQ and yet significant challenges with performance. This isn’t a lack of intelligence or effort. It’s a difficulty accessing information long enough to use it.
It’s not won’t. It’s can’t.
That small shift in language changes everything.
I’ve watched parents physically soften when they understand this. Shoulders drop. The edge leaves their voice. “Oh,” they say. “He’s not ignoring me. He’s overwhelmed.” That moment, more than any chart or consequence, is often where change begins.
The Myth of Consequences
One of the myths that runs deep in our field and in our culture is the idea that consequences teach behavior—natural consequences, logical consequences, consistent consequences. We see this play out in everyday moments. A child leaves the house without a coat on a freezing morning. They’re urged to “experience the natural consequence” of being cold so they’ll remember next time. But if the real issue is poor future thinking, difficulty shifting attention, or simply rushing out the door overwhelmed, the discomfort doesn’t build planning skills. It just creates more frustration.
Or a child forgets to bring home their math folder. The logical consequence is a zero. But if the child’s working memory is overloaded and transitions are chaotic, the zero doesn’t strengthen memory systems. It strengthens shame. Consequences only work when a child already has the skills to do something different next time.
If a child forgets their homework because of working memory challenges, or melts down because they can’t regulate frustration yet, adding a consequence doesn’t build the missing skill. It just adds stress. And stress is the enemy of executive function. No learning takes place when stress is in the room! What we often see happening under the rubric of “consequences” is escalation. Parents tighten control. Kids feel more pressure. Skills get worse, not better. From the outside, it looks like behavior problems. Up close, it looks like a nervous system under strain.
When I shifted my focus from fixing the child to educating and supporting the adults around them, something miraculous happened. Therapists told me their work felt easier. Not because kids stopped struggling, but because adults stopped interpreting every struggle as defiance or lack of motivation. “Why aren’t you trying?” became “What’s getting in the way right now?” “He knows better” became “How can we support this skill?”
That shift changes everything.
When parents understand how executive function shows up in daily life, they stop fighting their kids and start collaborating with them. They move into strategy mode: visual supports like a checklist taped near the door that says “Backpack. Lunch. Coat.” Routines such as a predictable 10-minute wind-down before homework begins instead of launching into it cold. Shared planning conversations on Sunday night to preview the week ahead and identify heavy days. Scaffolding that breaks a long writing assignment into “open the document,” “write one paragraph,” and “take a short break,” instead of expecting the assignment to emerge in one sitting.
The child no longer carries the burden of change alone. The system shifts with them.
What we’re missing, more often than not, is the lens. Love, logic, and intuition aren’t enough when we don’t first understand how neurodiversity impacts daily functioning. This lens means filtering behavior through an understanding of ADHD, executive function, brain development, and the nervous system rather than through assumptions about character or motivation.
***
Now, when therapists say, “The sessions go great, but nothing changes at home,” I don’t hear failure. I hear an invitation: To widen the frame and shift the lens. To bring parents into the process of a child’s therapy sooner. To spend less time motivating a child to do what their brain isn’t yet wired to do—and more time helping adults scaffold skills in everyday life.
Kids with ADHD don’t need more pressure. They need more understanding and support. And the expectation that children fix the broken systems around them isn’t just a terrible burden to place on them—it’s a burden that’s impossible for them to fulfill.
When the adults around them feel calmer, clearer, and more equipped, something remarkable happens. The whole family breathes easier. Not because the child is “fixed,” but because everyone finally sees what’s happening and understands what’s actually needed for a challenging situation to improve. And from there, real change becomes possible.
Cindy Goldrich
Cindy Goldrich, Ed.M., ADHD-CCSP, is a parent coach, educator, and trainer specializing in ADHD and executive function. She has trained therapists, educators, and parent coaches across the country to better support families navigating neurodiversity. She is the author of “8 Keys to Parenting Kids & Teens with ADHD” and the founder of PTS Coaching.