Enjoy the audio preview version of this article—perfect for listening on the go.
The most effective teacher I ever had in the field of trauma therapy wasn’t a trauma specialist, or a clinical expert, or even a colleague: she was a client, a deeply complicated woman, who initially scared the hell out of me.
Marisa came to see me in the early 1990s—about 10 years into my work as a therapist—because she’d begun to have terrifying obsessive thoughts about suffocating her 4-year-old daughter with a pillow whenever she heard the little girl crying. As she explained it, something about the child’s crying triggered almost intolerable feelings of rage and helplessness. I have to get her to stop screaming! I just want her to shut up! At the same time, Marisa felt deep fear and shame about these thoughts, insisting she’d never actually lay a hand on her child. At 35, Marisa was a highly intelligent woman in a stable marriage. She had a rewarding career as a librarian and was also the mother of an 8-year-old boy, who didn’t elicit such thoughts in her.
I was Marisa’s first therapist, and we quickly established a good rapport. She consistently showed up for sessions and followed—or tried to follow—the behavioral suggestions I knew to offer: taking time-outs when she felt stressed, learning to knit as a way to relax, reading the parenting books I suggested, listening to my advice about managing a crying child. She even brought her husband into a few sessions so I could work with them as a parental team. I knew she was trying hard, but these measures didn’t seem to be working. And because I didn’t want to let her down, I kept trying too.
As therapy continued, Marisa found the courage to share even more of her difficulties. By the sixth month of therapy, I’d learned that she was self-medicating with alcohol, cutting her herself, and struggling with medical maladies that ranged from chronic gastrointestinal upset to migraines to possible fibromyalgia. I began to feel uneasy. This is a deeply troubled woman with about 10 different diagnoses, I thought. I’m in over my head.
Then, during a session early on in our second year of therapy, it happened. Right there in my office, before my eyes, Marisa morphed into a different personality. As I sat frightened in my chair, she slipped off the sofa, sat cross-legged on the floor, and began talking like a 4-year-old. “Can we play a game?” she asked, her face bright with childlike anticipation. Before I could even think of a response, she followed up with, “Or can we color?”
Holy crap! What do I do? I thought in a panic. This was the first time I’d ever seen “switching” in real life—a behavioral manifestation of what was then called multiple personality disorder and is now known as dissociative identity disorder.
That session lasted well over an hour because, as a 4-year-old, Marisa couldn’t drive herself home, and I could hardly let her leave my office in that state. I got her to walk around the room, desperately trying to reorient her to present time and space, until the adult in her had sufficiently returned to know what to do with the car keys dangling in her hand. But my sense of inadequacy haunted me. The next time we met, I said, “Listen, Marisa, I have an inkling about what’s troubling you, but it’s something I have no expertise in treating. You deserve the best possible care, and I know just the therapist who can help you. I’d like to refer you to her.”
“No,” Marisa said, sitting up in her chair, her voice uncharacteristically firm. “I’m not going anywhere else. I want you to help me. So go ahead and read everything there is to read, talk to your supervisors, find all the resources you can, but I’m not going anywhere.” And so began my crash course in trauma therapy. I felt overmatched, but Marisa had been insistent. I feared that if I didn’t stay with her, she might not continue therapy.
Taking Up the Challenge
At that point in my career, I wasn’t completely ignorant about how to treat trauma. But the approach I’d been trained in during the late 1980s was based largely on the idea that clients like Marisa carried awful experiences that needed to be excavated and fully relived before they could be healed. Little, if any, attention was paid to the inner strengths that traumatized clients might reclaim if given half a chance. With the focus on all pathology, all the time, it was no wonder therapists tended to regard clients as one-dimensional bundles of dysfunction and pain.
And I could easily have come to see Marisa this way. After all, I soon learned that she’d been sexually abused for much of her life, from age 4 until 20. Her abusers included both of her parents, her sister’s boyfriend, and an unknown number of teenage boys who’d raped her when she was in a dissociated state. But by ordering me, in effect, to get my clinical act together and become an enlightened therapist, rather than a clueless one, Marisa revealed an aspect of herself that I hadn’t seen before. Here was a presumably “highly disturbed” woman exhibiting a solid sense of determination and willpower, as well as an acute awareness of what she needed to heal. Whatever her difficulties and however terrible her past—and it had been awful, indeed—she’d been at that moment capable of extraordinary self-advocacy, making it clear that her best chance of recovery lay in staying with me, in the trusting, authentic, and safe relationship we’d already established. My job, she essentially told me, was to stop wavering, bone up on the latest in trauma therapy, do my homework, and figure out how to help her.
The process was daunting, but I was game. I read every new book on trauma, attended every workshop I could find, and began to work with trauma experts who were on the cutting edge of the field in the early 1990s. I learned about the importance of creating a safe environment, taking the time to build a trusting relationship, assessing for and undoing cognitive distortions, and increasing external resources for support. But the prevailing belief was clients couldn’t fully heal until they fully remembered, even relived, their traumatic experiences. Throughout, it was Marisa who helped me understand how to pace the work, letting me know, often without tact, when I was going too fast. “Stop pushing!” she said once, cutting me off in mid-sentence. “When I say I’m not going there, I mean it, and you need to back off!” In other words, she had an almost uncanny sense of when it was safe or unsafe to explore a particular part of herself or address an emotionally painful memory.
And at a certain moment in our treatment, I had a kind of epiphany. Not only did I come to realize that she was the teacher when it came to her dissociative identity disorder, but that even the symptoms of her condition represented a kind of wisdom. Everything she grappled with—the thoughts, feelings, and behaviors that were pathologized in textbooks and held up as evidence of how troubled she was—were actually creative coping strategies that had kept her alive.
However frightening Marisa’s various parts seemed at times, it began to dawn on me that they weren’t fundamentally pathological. Instead, they were members of a self-created inner family that made it possible for her to function. Some parts pushed down her deep-seated rage so she could stay attached to her abusive parents and interact socially with peers. Other parts compartmentalized her memories of abuse so she could show up in school and concentrate on math and history. I began to view even her self-destructive behaviors—alcohol abuse and cutting—as creative attempts to both communicate her pain and distract herself from it when horrific memories bubbled to the surface and threatened to overwhelm her. Her symptoms were lifesaving emergency measures. And I began to regard her with admiration, even awe, for the strength of mind and soul that allowed her to survive.
This new way of looking at Marisa began to carry over into my work with other clients who’d suffered seemingly insurmountable trauma. Rather than asking myself, What are their diagnoses? I found myself wondering, What did they do to survive? How did they not jump off a bridge by the time they were 10? This was a new form of questioning for me. My emphasis was shifting from what was wrong with the clients to what was right with them. What inner strengths have kept them going despite what’s happened to them?
I was excited and energized by this shift in my thinking and practice. At the same time, I felt anxious. If I nudged clients away from focusing only on their trauma narratives, would I be minimizing or invalidating their stories and pain? Could I focus on their strengths and still find a way to honor the legitimacy of their horrific trauma? I wasn’t really sure how to navigate this new balancing act. All I knew was that the way I’d been working with clients, focusing solely on their trauma, felt heavy and stuck. The truth was, my clients often left sessions feeling either angry or deeply sad.
Wasting Away
Around this time, 16-year-old Kathy came to me for treatment. She was a nervous, notably thin girl, who wore her silvery-blond hair in a ponytail. Her mother was severely depressed and relied on alcohol for self-medication. Her father, an emotionally distant workaholic, denied his wife’s drinking problem. An only child, Kathy felt responsible for her mother’s chronic despair. “I spend a lot of my time either trying to cheer her up or not make it worse,” she said. She also expended tremendous energy attempting to predict or sidestep the emotional rollercoaster that accompanied her mother’s binges.
Despite all the family dysfunction, Kathy was the identified patient because she struggled with anorexia. It went unnoticed for a while because she was an honor-roll student and the captain of three sports teams. Finally, after she’d lost close to 20 pounds, her basketball coach had taken her parents aside and persuaded them to take her to a therapist.
When we first began working together, I kept the focus on her eating disorder symptoms and helping her gain weight. But just as Marisa had channeled her inner wisdom to find the courage to tell me what she really needed, Kathy let me know when I was on the wrong track. So one afternoon, midway through a session that was clearly going nowhere, she yelled, “This is a huge waste of time! All you want to talk about is calories, and all you try to do is convince me to eat more. It’s stupid!”
“So talking about eating is a waste of time,” I mirrored. I was just stalling for time. In the awkward silence that followed, it dawned on me that what I was hearing wasn’t resistance, but courage and insight. My frustration softened. “I’m glad you spoke up,” I said. “That took guts! And I don’t want therapy to be a waste of your time. Do you typically let people know what you do or don’t want?”
Kathy seemed startled by the question. Then she gazed directly at me and said, “Do I let people know what I want? Now that would be a waste of time!” At that point, we stopped talking about food and started talking about how invisible she felt in her family. In time, it occurred to me that Kathy was creatively reenacting that invisibility through anorexia, and her symptom of restricting calories started to make sense to me. Maybe it was a way for her to communicate a lack of emotional nurturance, a nonverbal declaration of her feelings of loss and futility.
Admittedly, it felt scary to go beyond Kathy’s eating disorder diagnosis and start thinking about her skill in navigating her family’s dysfunction. At the same time, it would clearly have been a mistake to focus only on her pain, because she was also marshaling the energy and initiative to create an exit strategy. “Doing well in school and sports means I can get a scholarship to college,” she told me. There were certainly a lot of issues and symptoms to reconcile, but Kathy had tremendous potential. Again, I wondered where to put my focus. Then I got it: I didn’t need to agonize about whether I should validate trauma or highlight strength. I realized that I didn’t have to choose a side.
As I embraced the reality that both perspectives were valuable, I started working with my clients differently. I understood their symptoms as both painful and traumatic and creative and lifesaving. By holding that “both/and” thinking, I could bring more hope to the work. Together, my clients and I began to become curious about their innate abilities and about other, more affirming aspects of their lives. I started to talk less and listen more, and what I heard confirmed that my clients were more than their trauma—much more. Not only were they simultaneously struggling and growing, but in many cases, their growth seemed to be the byproduct of that very struggle.
Taking Up the Baton
As my therapeutic lens kept expanding, I started seeing Judy, a 45-year-old woman whose sister and three children had been brutally murdered by the sister’s husband. Judy blamed herself for not being able to protect her loved ones from their abuser. In our early sessions, she cried uncontrollably, saying almost nothing. Outside my office, she was haunted by nightmares, ate little, and barely functioned at her job. “It’s like he murdered me, too,” she whispered over and over. “I have nothing to live for.” Although I often felt inadequate in the face of her despair, I noticed that Judy showed up early for every session. Every time I opened my waiting room door, she was there. I felt a glimmer of hope.
Nonetheless, she continued to be lost in grief, self-blame, and even a wish to die. I realized I had to do more than be a compassionate presence. I had to take a more active role in therapy. What I had to become, I finally understood, was a conductor.
I came to this realization six months into therapy when Judy offhandedly said, “I’m thinking about planting a tree to honor my family.”
“Wait, wait, wait,” I found myself saying. “Slow down and notice that. What did you feel in your body when you said you wanted to plant a tree?” I wanted Judy to stay with her seemingly offhand remark because I heard it as a statement about taking her trauma and doing something meaningful with it.
Judy dismissed my invitation. “It’s not that important,” she shrugged. “It’s just something that crossed my mind.”
But in my emerging role as a conductor, I used a verbal baton to keep her focused on the note she’d just played, shifting the pace from fast to slower, as you would a piece of music. “I want you to stay with it,” I said. “It’s really powerful. It’s important.”
Comments that Judy made under her breath in the first few minutes of a session—“I was thinking I might start going to films again at some point” or “I heard a joke at work today and I actually laughed”—became the focus of our whole session. This idea of pausing the music, reflecting it back, and then inviting Judy to notice what she felt in her body, the images it conjured, the emotions it tapped into, allowed her to not only notice moments of grief, anger, and fear, but also hope, playfulness, and a sense of the future. Gradually, she was starting to believe there was more to her life than her terrible trauma.
For me, the notion of conducting a kind of therapeutic symphony began to resonate more and more. I saw my clients’ multifaceted experiences, thoughts, and emotions as components of an orchestra. In Judy’s case, grief would swell like a string section; guilt would boom and crash like percussion instruments. Sometimes, resiliency and hope would emerge as a more tentative woodwind section. I realized that much of the time Judy experienced these emotions as internal chaos, each orchestral section vying to be the loudest, and often playing vastly different arrangements of the same tune simultaneously. I want to move forward with my life competed with But I’m afraid if I stop grieving, I’ll be leaving my family behind. At times, it was more cacophony than symphony.
Of course, my ultimate goal for Judy and my other clients was to allow them to become the conductors of their own inner orchestras. But at first, they needed me to model this process of consciously tuning in to each feeling and thought, honoring and validating it, and then creating a space for other kinds of experiences to be heard. As with the instruments that make up an orchestra, we needed to explore what each could contribute individually, tuning into the humor, creativity, hope, vision that emerged as we brought fuller, more resonant harmonies into the room.
Bringing in the Orchestra
As I continued in my work as a trauma specialist, I often heard Marisa’s words in my head: “Read more, go to conferences, study with mentors so you can figure out how to help me.” And I did. Profoundly inspired by Richard Schwartz’s Internal Family Systems model, I invited Kathy to access and bring forward the part of her that felt compelled to starve. She then put that part in an empty chair, Gestalt therapy-style, conversed with it, and slowly began to experience compassion and empathy toward that part.
With Marisa, I used strategies from Focusing and sensorimotor psychotherapy while also working with movement, body sensations, and breath to process her painful memories of sexual abuse. With my encouragement, she drew images of safe places and wrote poems celebrating her 4-year-old daughter as well as her wounded 4-year-old self. Meanwhile, Judy processed her ambivalence about wanting to stay connected to her murdered family while wanting to live her life to the fullest again. One way she did this was journaling with both her dominant and nondominant hand—the left hand processed her grief and fears while the right expressed a desire for healing and forward movement. This allowed her to give voice to those equally valid needs.
Working creatively seemed to energize many of my traumatized clients, in part because they were already creative, having invented all kinds of strategies for safety and survival. Now they were using their imaginations to move beyond their pain and even find ways to make meaning from horrific events. Marisa, for example, developed a plan to speak at local high schools to educate teens about rape. She said to me, “I’m going to do everything in my power to help spare girls the terrible trauma I experienced.” And as Kathy continued to struggle with anger about her mother’s alcoholism, she allowed herself to imagine a future freed from her family’s dysfunction. “Whatever it takes, I’m going to college—going away to college,” she announced. “I’m gonna become a psychologist. Maybe I can help other kids like me.”
After abandoning the church for most of her adult life, Judy gave herself permission to, as she put it, “shop around to find a church where I can feel safe and supported because I need to believe that there’s a heaven and my family is there acting as my guardian angels.” All three of these trauma survivors were still in tremendous pain, yet they were growing, expanding their self-narratives. They were beginning to conduct their own life symphonies.
Post-Traumatic Growth
As I continued to bear witness to similar processes with other traumatized clients, I stumbled upon a paradigm called positive psychology, developed by University of Pennsylvania psychologist Martin Seligman, that was grounded in research exploring the qualities that allowed individuals to thrive in the face of adversity. Contrary to his original clinical assumptions, Seligman discovered that not everyone responded to trauma with a pervasive sense of helplessness. For some, the byproduct of trauma was significant growth, hope, and even empowerment. This clicked for me: I was witnessing it in my own practice. Further, the research found that clinicians could nurture this kind of growth by helping clients shift into positive emotions and thoughts, and encouraging them to pursue supportive relationships.
Seligman’s emphasis on clients’ strengths and their ability to learn from and transcend trauma opened up a new way of thinking about the aftermath of trauma—something University of North Carolina at Charlotte psychologists Lawrence Calhoun and Richard Tedeschi called post-traumatic growth (PTG). While acknowledging the emotional, somatic, and cognitive impact of trauma, Calhoun and Tedeschi proposed that trauma wasn’t necessarily irreparable, nor did it cause all clients permanent psychological and emotional distress. Instead, the PTG model presented the possibility of growth through struggle. Insight and healing could occur even in the midst of painfully devastating experiences—and even because of them.
One afternoon, after years of working together, Marisa sat down in my office looking tense and agitated. “I often come home from giving talks to kids on the dangers of rape and feel good about what I’ve done,” she said. “But then I get hit with this wave of anger and sadness. It brings stuff back up for me and I want to start cutting again.”
I was caught off guard. “Is it possible that it’s too soon in your healing to be doing this great work at the schools?” I asked. “Maybe it’s too triggering for you.” I thought I was being helpful by giving her permission to slow down.
Marisa looked scornful. “Jeez, I never thought this would be a picnic! Come on, Lisa! I just need more tools to handle it when I do get triggered!” Whoops. As my client reminded me, this work was not about eliminating her discomfort, but about giving her concrete ways to sit with it while continually reminding her about her capacity to navigate through it. As I used my conductor’s baton, I needed to listen more carefully and be more respectful of Marisa’s dissonant notes as well as her melodic ones.
As I worked with other clients from a PTG perspective, I began to listen for experiences that showed a willingness to reach out to others—an important element of PTG. Two years into treatment and after a lifetime of secret-keeping, Kathy said, “Last Thursday, I confided in my coach and two of my teammates about my mother’s drinking. I’m sick of pretending that nothing’s wrong with my family and my eating disorder is the only problem. Screw that! She’s an alcoholic, whether she admits it or not.”
“How did it feel to break that silence and trust other people with such intimate information?” I asked.
“Scary at first,” she admitted. “But I started to realize that not everyone is screwed up like my parents are. A lot of people out there care about me and won’t judge me. And I found that out. My coach and teammates have been really supportive. In fact, they’re amazing! It’d be stupid not to let them in.”
Kathy’s new willingness to disclose reflected her growing belief that others were inherently good—a belief that often gets challenged when a client feels betrayed by an abusive or neglectful caretaker. But as she moved into PTG, Kathy was expanding her view of the world and beginning to reconnect with the idea that kind and safe relationships are possible. She was no longer a lonely soloist; she was creating her own community ensemble.
Seven years into therapy, even as Marisa continued to navigate many ups and downs, she began to feel more compassion toward herself, her fragmented parts, and remarkably, even her abusers. “My parents were horribly abused themselves while they were growing up,” she told me. “I’m not making excuses for them. It’s just that I’m starting to understand that there are generations of victims and pain in my family. My parents were clueless. Yeah, they should’ve learned how to parent better, but they had ninth-grade educations, no money, no way to get therapy.” She sat up straighter in her chair. “I know that I’ll never let my kids suffer the way I did. The cycle of abuse and ignorance stops with me.”
In a visible shift from PTSD to PTG, Marisa took the quilting needles she’d used for years to cut herself and began using them to make beautiful quilted bedspreads for children in homeless shelters. She was setting free the parts of her that had punished her body and channeled her pain through self-destructive behaviors.
Judy also forged her own path toward growth and healing. After several years of feeling “numb and emotionally dead,” she became determined to attach meaning to her tragedy and pay it forward—important indicators of PTG. When traumatized individuals express a desire to pay it forward, they are not only coming to terms with their own traumatic experiences, but wanting to become a source of inspiration and hope to other survivors. In Judy’s case, that meant sponsoring events to raise money for domestic violence programs and shelters in her city. In a single year, she raised 200 thousand dollars. Despite an intense fear of public speaking, she went on to tell her story to legislators in her home state and singlehandedly got a new law passed: anyone indicted for domestic violence could no longer possess a rifle, the weapon that had been used to wipe out her family.
Judy’s passion for advocacy continued to grow. After weeks of tweaking her script in my office, Judy appeared before the US Congress and spoke with the Vice President of the United States to get stricter laws passed to protect victims of intimate partner violence. “I can’t bring my family back,” she told me in tears. “But I have them with me every time I testify. And when even one person becomes more educated about the impact of domestic violence, then maybe a life has been saved.” Speaking out about domestic violence also changed Judy’s narrative about herself. She stopped describing herself as an awkward introvert and recognized that expressing emotions was a sign of her strength.
—–
In my 32 years of trauma work, I’ve learned to see my clients as genuine heroes—wise, brave, and creative at the same time that they’re holding intense pain and sorrow. And I’m honored to help conduct their orchestra of inner parts until they can do so on their own. I know I can’t play their instruments for them, but I can guide and inspire them, hoping that phrase by phrase, measure by measure, they can begin to create their own music.
In my office, I’ve discovered how to listen closely to the complex notes my clients play—sometimes the strings are weeping; other times the percussion section is dominant, insisting on being heard. The melodies might be reclaimed from the past, or they may be brand new compositions, but what’s most important is that my clients find within themselves the capacity to create inner music that inspires and heals them. And when they do, I pass the baton, feeling privileged to have witnessed them move from being trapped by intense feelings of grief, loss, and victimization to becoming maestros of their own lives.
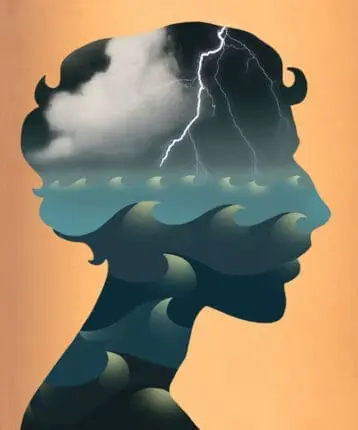
Illustration © IllustrationSource.com/Fanatic Studio
Lisa Ferentz
Lisa Ferentz, LCSW-C, DAPA, is a recognized expert in the strengths-based, de-pathologized treatment of trauma and has been in private practice for more than 35 years. She presents workshops and keynote addresses nationally and internationally, and is a clinical consultant to practitioners and mental health agencies in the United States, Canada, the UK and Ireland. In 2009 she was voted the “Social Worker of Year” by the Maryland Society for Clinical Social Work. Lisa is the author of Treating Self-Destructive Behaviors in Trauma Survivors: A Clinician’s Guide, 2nd Edition, Letting Go of Self-Destructive Behaviors: A Workbook of Hope and Healing, and Finding Your Ruby Slippers: Transformative Life Lessons From the Therapist’s Couch.