About once a month, a teacher, school counselor, or pediatrician refers a child to me for evaluation and treatment of attention deficit hyperactivity disorder (ADHD). Often someone has administered a Conners teacher or parent rating scale that presumably justifies the diagnosis, or the child has already been diagnosed with ADHD and has taken medication without symptom improvement. Such children commonly exhibit troublesome symptoms, including agitation, moodiness, hyperactivity, and distractibility, so I understand why they were referred to me. But what I can’t understand—and have become increasingly emphatic about pursuing—is why professionals diagnose and treat ADHD symptoms without first trying to understand the causes of those symptoms.
In my view, there’s an epidemic of misdiagnosis of ADHD in young children. Yes, school personnel are overwhelmed by the number of children whose poor concentration make it difficult for them to learn, and a number of likely explanations have been offered for the apparent increase in hyperactivity and inattention in children. Class sizes are bigger than they once were. Music, art, recess, and physical education—activities that used to provide a break from routine—have nearly been eliminated in many school systems. Children spend too many hours on video games to the exclusion of creative, unstructured play, and they don’t get the amount of physical exercise that contributes to healthy brain development. Lack of adequate sleep also contributes to poor mood and focus, as do the challenges faced by children of substance-abusing or addicted parents.
Schools and physicians are aware of some of the above, but they don’t seem to understand the ways in which trauma leads to symptoms that resemble ADHD. Thus, we all need to ask the right questions and dig a little deeper in creative ways to find out what may be troubling the child so that our treatment is effective and not just a surface remedy for a misdiagnosis. In other words, it’s crucial to figure out why a child is tuning out, having trouble concentrating, and being moody and hyperactive. A child living in dangerous chaos, for example, has to find ways to cope and adapt, and the resulting stress-based behavior can sometimes mirror ADHD symptoms. To complicate matters, many children referred for suspected ADHD are in preschool, kindergarten, or early elementary school and are so young they don’t yet have the verbal and conceptual skills to tell us what’s going on in their lives. Thus, therapists need to get a thorough family history, engage the child in play activities (e.g., art, stories, puppets, sand play, and dollhouse), and observe the child’s play for clues about the cause of the symptoms. Only then can we form a plausible hypothesis, develop a plan of care, and match interventions to a child’s issues.
Getting to Know Ella
Five-year-old Ella, who’d just started kindergarten, was brought to my outpatient treatment office by her mother at the request of her first-grade teacher. At school, Ella would talk out of turn, get out of her seat without permission, and boss other children around.
“Her teacher thinks Ella has ADHD and should be on medication. He says she’s behind the other children and can’t pay attention,” her mother told me. “I don’t know what to think.”
To start, I began collecting a life-and-developmental history to help me rule out ADHD. In other words, if Ella actually had ADHD, there’d be no other factors to account for trouble sleeping, difficulty completing or following tasks in school or at home, impulsivity, and hyperactivity. I also wanted to rule out conditions that include ADHD symptoms, such as autism spectrum, depressive disorder, post-traumatic stress, complex stress, anxiety, and adjustment disorders.
I started by inviting Ella to play with the toys and puppets in my office so she could stay occupied while I spoke with her mother. Our conversation revealed that she was tired of Ella’s “bad attitude,” yet concerned about her daughter’s nightmares, fear of sleeping in her own bed, waking during the night, and frequent tearful and angry outbursts. She found her daughter’s high-intensity behavior exhausting and gave up quickly when Ella didn’t listen to her. I wondered if her lack of energy might indicate depression, especially since children of depressed mothers have to work so hard to get their mothers’ attention that they can show symptoms of anxiety and ADHD. If that proved to be the case, I’d refer the mother for treatment of her own.
Meanwhile, Ella offered a constant commentary on her exploration of the office toys; however, when she felt excluded from my conversation with her mother, she became provocative, intrusive, and pouty. She answered questions I directed to her mother about Ella’s sleep behavior, school performance, and noncompliance with chores and rules. I suspected that this little girl wanted to be in charge, in control, and independent. I wondered what in her life might have led her to mistrust and ignore her mother’s directions. Ella’s behavior mimicked some symptoms of ADHD, but she seemed too attentive and intentional in her actions for the diagnosis to fit.
Because Ella was more watchful than most ADHD children, even though her eye contact was intermittent, I began wondering about the source of her vigilance. I noticed times when she’d tune out briefly (stare off and make no comment) or quickly change the subject. As I watched for a pattern to these episodes, it became clear that the tuning out increased when we said anything about her biological father, who was divorced from her mother and in jail. The subject of her father seemed to increase Ella’s level of physiological and emotional arousal. I suspected that Ella’s inattention and high arousal might actually be dissociation or avoidance related to her father.
When I finished my interview with the mother, I turned to Ella to ask why she thought she was coming in to see me.
Without hesitation, she said, “I’m bad at school and I don’t like my teacher. I won’t sleep in my own bed, and mommy says I have a bad attitude. My daddy is in jail for hurting mommy and me.” She paused and added, “Dr. Pat, my daddy lied to me. He took me away, and he wouldn’t let me go home to my mommy.”
Aha! There it was—a clear clue as to why Ella felt so powerless and needed to take charge. Something traumatic must have happened to her and her mother at the hands of her father. I knew I needed to explore what had happened, see how it was affecting the relationship between Ella and her mother, and help them process the trauma. For this to happen, both Ella and her mother would need to be involved in treatment. Her mother’s anxiety was palpable and contagious for Ella. What Ella needed was a strong, take-charge, nurturing protector. Instead, Ella seemed to sense her mother’s victim stance and acted out to communicate her fear and vulnerability. When behaving provocatively and making demands, Ella was pushing and challenging her mother to take charge.
At this point, I realized that Ella was a brave little girl who was just as worried about her mother as her mother was about her. By volunteering information about her father’s mistreatment of her and her mother, she showed she was purposely recruiting me as a partner to fix her and her mother’s shared problems. She displayed many traits of insecurely attached children whose parents are fearful, anxious, or depressed. Such parents are inconsistent in caregiving, and their children have to take care of themselves or make increasingly high demands on parents to notice them.
It turned out that Ella had been abducted by her father, and when her mother had gone to retrieve her they’d both been physically assaulted. When her father was subsequently put in jail, Ella’s symptoms emerged. Ella’s mother began showing symptoms of post-traumatic stress as well: she was irritable and short with Ella, lacked patience, and found herself being critical and negative instead of comforting or nurturing. She didn’t understand that Ella was responding out of fear, not defiance. Since Ella’s mother could see that she was sometimes contributing to her daughter’s problems, she agreed to participate in treatment.
For Ella’s part, like most traumatized children, she had trouble talking about her feelings and reactions to what had happened with her father. She said it was her fault that her mother had gotten hurt, and she feared her father would come back and hurt her again. At the same time, she wanted to be the one who’d magically change her father into a “nice daddy” and be worthy of his love.
Young children almost always have ambivalent feelings toward an abusive or neglectful parent. Early on, Ella’s play indicated that she experienced loss, love, sadness, anger, and fear toward her father. She used the sand tray to enact power and control scenes where frightened victims fought back against a “mean bad guy.” The dollhouse became an orphanage for babies and children whose “mean daddies” were in jail, and they cried for them at night. I wanted to help Ella express her feelings and understand that she wasn’t responsible for her father’s behavior. I planned therapy activities that would allow Ella to “feel felt” by her mother and allow her mother to show empathy and protectiveness. She also needed to trust that her mother could handle whatever might happen and keep her safe. As her mother became less anxious and worried, I believed that many of Ella’s symptoms would spontaneously dissipate.
To this end, I taught them relaxation and breathing practices early on to help them lower their anxious arousal. We ended most sessions with our eyes closed, listening to a Tibetan bell bowl and holding stones to warm them. With practice, Ella became able to remain still and quiet, letting her fear and anger move into the stones. Body–mind approaches are helpful in trauma work, since calming the body and its arousal is essential for self-regulation. Together, she and her mother practiced breathing at bedtime, and their anxiety subsided. Also, claiming it chased away her nightmares and allowed her to sleep in her own bed, Ella slept with her stone at night.
Within a few weeks, it seemed time for Ella and her mother to process the trauma more actively. Over a six-month period, I worked with them using stories as well as fear-reducing and symbolic play-based, expressive, and cognitive behavioral techniques. Generally, I pulled her mother in as a helper. For example, when Ella revealed she thought the assault was her fault, I read a story about self-blame, and then identified a puppet that blamed himself for getting hurt. Afterward, I asked Ella, “Is it his fault? Why not? Who should’ve been in charge? Why do you think he’s blaming himself? I wonder what you could tell him to give him the facts and show him he’s not at fault.” Then Ella and her mother came up with a list of reasons why it wasn’t his fault. Together, they talked to the puppet and corrected his faulty beliefs.
Taming the Alligator
Metaphorical stories and puppet play (modeling and enactment) were powerful change agents for this dramatic, engaging child. I provided a story or theme idea for most play sessions, and Ella’s creativity propelled the action, in which she revealed her feelings and concerns. As Ella opened up through stories and puppets, her mother showed increasing empathy and offered more verbal encouragement and affectionate touch.
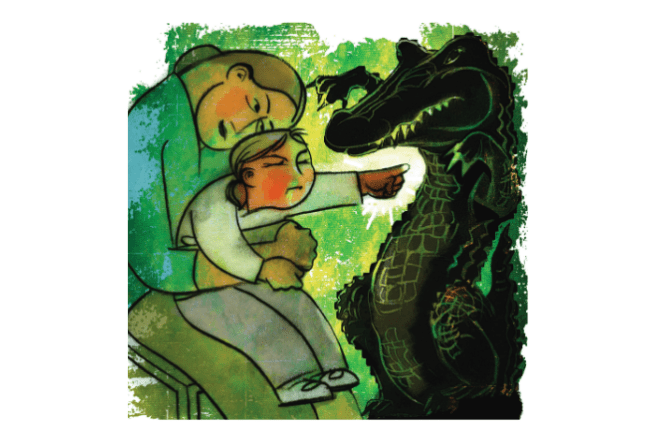
During a particularly pivotal session about three months into treatment, Ella asked to do a puppet show and took charge of it. She selected an alligator perpetrator, a kangaroo caregiver, a small multicolored frog victim, and a colorful rainbow dragon as a helper. The characters helped her tell and process her trauma story, and the parallels to her family were obvious. In her show, the alligator puppet promised to be nice, but then started biting the other puppets.
Ella shook her finger at him: “You need to tell the truth and stop telling lies. You have an anger problem! You need to change and be nice.” She then wrapped his long snout in duct tape. Turning to her mother and me, she said, “He has an anger problem. He needs to calm down and control his temper. We should put him in jail for biting.”
Ella’s mother agreed, and together they put the alligator in jail. We agreed that we should not be mean to him; rather we could feed and talk to him from a safe distance.
When I asked Ella how the alligator could learn to control his anger, she replied, “Let’s teach him to calm down.” She handed her mother and me one stone each and said to the alligator, “You need FIVE stones. You have BIG ANGER!” Shoving five stones inside the taped snout, she then taught him how to breathe and rang the Tibetan bell bowl. “Close your eyes and relax,” she instructed. When the ringing stopped, Ella announced, “The alligator can stay in jail until he decides to be nice.”
Later in the session, Ella looked up from drawing on the dry erase board and said, “I’m going to the jail to tell my dad to stop being mean. Then he’ll change and be nice.”
Ella clearly had ambivalence about her own anger at her dad since, even though she feared him, she still loved him. To help her make sense of this ambivalence and gently challenge her magical thinking about change, I commented, “Ella, I know you love your dad and want him to change. Sometimes people change, and sometimes they don’t. They have to be sorry for what they did and really want to change.”
Ella went over to the cage where the alligator was being held. She asked him, “Are you sorry for what you did? Do you want to change?”
I spoke for the alligator and said, “Please let me out. I’m sorry I bit you. I promise to be nice this time.”
Ella said to me, “He says he’s sorry, and he promised to be nice. Can we take off the duct tape and let him out of jail?”
I decided to pull in Ella’s mother at this point and asked what she thought. She took Ella’s hands and said, “It’s too soon to do that. I don’t think he’s sorry. He doesn’t think he did anything wrong. He promises to be nice, but he doesn’t change. I don’t think he really wants to change. I’m going to keep you safe, and I won’t let him hurt you.”
Ella thought for a minute and said matter-of-factly as she crawled into her mother’s lap, “He’s always been mean. He needs to stay in jail. And leave the duct tape on. He’s not ready to come out yet.”
So were we talking about her father or the alligator? Obviously both, but in conquering the alligator, Ella had come to grips with her father’s behavior.

It’s worth noting that over time, the family system had changed: Ella’s mother had benefited as much as her daughter from the relaxation and healthy coping skills I’d taught them. The treatment had helped her recognize her own struggle with anxiety and depression, and she’d come to see how this struggle had affected Ella’s functioning. Thus, she asked her doctor to prescribe an SSRI antidepressant, and was demonstrating more nurturing behavior toward Ella. She’d become a safety advocate for Ella and herself, and as a result, Ella trusted her to be in charge and protect her.
During our final session, I complimented Ella on her hard work and progress and said to her mother, “She’s doing well in school. She can sit still and pay attention. She has no more nightmares and is sleeping in her own bed.”
At this point, Ella interrupted quietly and said, “Dr. Pat, I’m not as afraid of the alligator anymore either. My dad got out of jail, but I can’t see him until he gets better with his anger.”
This case had a good outcome, but I wonder what would have happened if the school’s diagnosis of ADHD had guided Ella’s treatment. We need to be mindful of the possibility of trauma when a child presents with symptoms of ADHD. Child abuse, neglect, and domestic violence occur in all types of families, and we have to do a better job asking the right questions and digging deeper—for the sake of children like Ella.
Case Commentary
By Martha Straus
The differential diagnosis of young children can be challenging even for the most trained and attentive clinician. After all, a five year old has a fairly limited repertoire for communicating distress. Plus, as Pat Pernicano wisely notes in her compelling case study, oppositional behavior, sleep issues, irritability, tantrums, bossiness, and hyperactivity could all be symptoms of a single,or comorbid diagnosis, including ADHD. These same behaviors, however, might also describe a five year old going through a tough patch—a normative, and perhaps transient, response to developmental or environmental stressors. Compounding the issue is the fact that traumatic experiences are more common in communities with fewer resources to treat it, so trauma is inevitably underdiagnosed.
The gold standard for making an ADHD diagnosis includes collecting as many data points as possible, such as a solid developmental history, interviews, assessment, play evaluation, observations, rating scales, and other reports. Such a comprehensive diagnostic assessment makes tremendous sense, and it would assist in sifting out the underlying stressors for young children who are challenging and challenged in those sit-and-be-quiet kindergartens. But it’s hugely expensive. Few children have the benefit of the skilled, costly, and time-consuming protocol that Pernicano describes and so deftly pursues.
I wonder what might be different if schools and physicians did understand the way that trauma can show up as inattention? Would these kids then get competent evaluations? Would classrooms accommodate their special needs for compassionate support and predictable activity? Would they get to go to play therapy?
In terms of play therapy, I particularly admire the combination of directive and nondirective techniques in Pernicano’s intervention. She’s able to make a strong and useful alliance with the mother while engaging in thoughtful dyadic play therapy. This approach has the wonderful advantage of modeling and practicing supportive parenting techniques, relaxation strategies, and coregulation. Ella’s mother was then better able to guide her within the healing metaphors of play and set safe limits for both of them.
Illustration © Sally Wern Comport
Pat Pernicano
Pat Pernicano, PhD, is a licensed psychologist in Louisville, Kentucky. She teaches part-time at Spalding University and treats children and families in Clarksville, Indiana. She wrote Using Trauma-Focused Therapy Stories: Interventions for Therapists, Children, and Their Caregivers.
Martha Straus
Martha Straus, PhD, a professor in the Department of Clinical Psychology at Antioch University New England, is the author of No-Talk Therapy for Children and Adolescents, Adolescent Girls in Crisis, and Treating Traumatized Adolescents: Development, Attachment, and the Therapeutic Relationship.