Enjoy the audio preview version of this article—perfect for listening on the go.
The clients I saw in my practice last week were typical of my ordinary caseload. There were couples in violent relationships, an internist who’d sexually abused patients and nurses, an agitated combat veteran just returned from Afghanistan, and a woman who’s spent nearly 20 years cut off from her family and friends because her abusive and jealous spouse keeps her completely isolated. There were also clients whose traumas were less obvious and dramatic but still shaping the way they handled the stresses and conflicts in their present lives. Whatever the differences in presenting symptoms, the common thread in almost all the cases I see is a legacy of complex trauma as a result of relational violence or severe neglect within a family.
Such cases have been the focus of my work over the past 35 years, a period in which the trauma field has seen the emergence of powerful therapeutic innovations like eye movement desensitization and reprocessing, Somatic Experiencing, dialectical behavior therapy, and Internal Family Systems, as well as many major advances in our understanding of the brain and the neurobiology of trauma. Clearly, we’ve made important strides in our ability to help overwhelmed and hopeless people overcome the stigma previously attached to trauma symptoms, learn new thinking and self-regulation skills, and even find a new sense of restored well-being—at least for the period of time that they’re with us in our offices.
But then they go home, and far more often than we’d like, when they’re back in their daily lives with family, friends, and coworkers, they don’t do so well. In fact, no matter what progress they make in therapy, once they leave the safe, rarified space we provide them in our treatment rooms, they frequently fall right back into the same old patterns of negative emotion and dysfunctional relationships.
Let me give you an example. Lucy, a therapist I supervise, recently came in to discuss a difficult case. Her client, Abbey, a 46-year-old woman, suffers from severe anxiety and depression, abuses prescription drugs, purposely harms herself by hitting herself all over her body and head, frequently quits or is fired from jobs, and regularly alienates the few friends she has. Like many trauma sufferers, she’s easily triggered by her interactions with just about everybody she knows, especially her husband and two teenage children, who she says are “miserable, nasty human beings.” At home, she fluctuates between furiously attacking them—yelling hateful remarks, throwing things—and withdrawing into a sullen shell.
During sessions, Abbey dissociates while talking about her life, past or present. But through Lucy’s guidance and skill, she’s learned and practices many mindfulness techniques that have enhanced her ability to recover and bring herself back into her body when she shuts down. Most days when Abbey leaves therapy, she’s calmer, exhibits some genuine insights into herself and her problems, and often seems to be discovering an embryonic, but real, sense of inner selfhood. By the next session, however, it’s as if she has amnesia for all that transpired in the previous week. So she routinely begins each session, week after week, in varying states of anger, despair, dissociation, hyperanxiety, or rock-bottom depression.
By any measure, Lucy is an accomplished, well-trained therapist, proficient in integrating a range of therapies into her practice. And Abbey is a willing client: she meditates daily, takes the appropriate medications, cooperates fully in sessions, and practices many of the skills Lucy has taught her. Apparently, Abbey likes Lucy very much, and the two have a warm, mutually trusting working relationship—but the therapy is still stuck.
“Help!” Lucy said to me during our consultation. “I don’t know what else to do. Why isn’t she getting better in her outside life?”
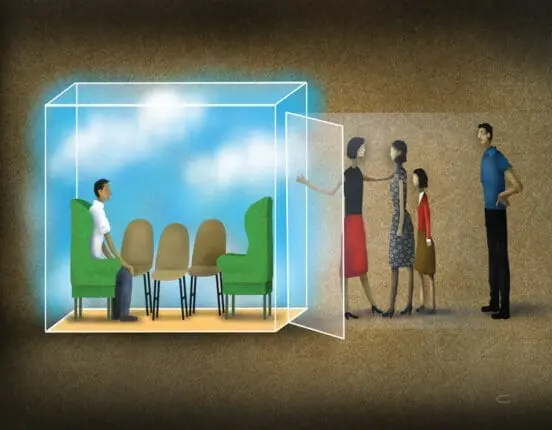
Most clinicians believe that the benefits of individual therapy should naturally transfer to the rest of a client’s life. But what if that’s not necessarily true? What if the positive interactions a person has with a therapist in the “inside” world of the consulting room don’t translate into the language of relationships conducted in the “outside” world of the person’s everyday life?
In therapy, clients feel—often for the first time—truly seen, heard, and understood. It’s no wonder they might think, with a sparkle in their eye, that if only their therapist was their spouse (or parent or friend or child), their lives would instantly be better. It’s no wonder they might scream in the middle of a fight at home, “Well, at least my therapist understands me!” So why are we surprised when real-life spouses, parents, friends, or children begin to see us—the all-loving therapists—as threats to the marriage, the family, the friendship? After all, therapists—yes, me included—can unwittingly play into this ultimately damaging process.
Demonizing the Family
Steve, an account executive with a major advertising firm, came to me suffering from severe anxiety. Early in life, he’d been sexually abused by a neighbor and had witnessed the death of his sibling in a drunk-driving accident. Now he imagined catastrophes every time any person in his family would leave his sight, and he’d cope with his overwhelming feelings by spending hours watching porn and gambling on the Internet.
In my office, he complained that his wife was making his life even more miserable by accusing him of being cold, distant, and incapable of ever really loving anybody. But as much as I tried to convince him to bring her in for a couple’s session, he refused, explaining, “This is the only place I can talk without being yelled at. If she comes in, she’ll just take over and blame me for everything.” Despite my training as a family therapist, over time, Steve’s description of her continual heckling became so convincing that, without quite acknowledging it to myself, I began to adopt his view of her as mean and unrelentingly critical.
I suspect that something like this dynamic occurs far more often than we admit. And I suspect that it fuels the client’s experience of returning home—especially after an enlightening hour alone with a compassionate, soothing therapist who hangs on his every word, every sigh—to find that home seems more like a place of conflict, disappointment, uncertainty, and even danger than ever before. After having his wants and needs being given weight and importance by the therapist, the client must face, all alone, those immovable other people at home who have their own wants and needs—often at odds with the client’s. It shouldn’t come as a surprise then that a client like Steve would come to firmly believe that no one at home understands him, feels for him, or has the patience to just listen to him.
Meanwhile, family members instantly pick up on the invidious contrast in the client’s mind between the wonderful therapist and their un-wonderful selves. Steve’s wife, for instance, might look at him, back from the therapeutic love-fest, and wonder, “Is he talking about me in therapy? What’s he saying? Why does he always seem to be in a worse mood when he gets home? Does he blame me for everything?”
To some family members, the client’s therapy can even feel like a kind of infidelity, triggering their own insecurities, anxieties, and even panic. As they see it, my mother, my sister, my husband, my child is experiencing a powerful attachment to someone outside the legitimate home ties. In essence, the client implicitly communicates to the therapist, Only you understand me; only you are there for me, which the family members pick up on as a rejection of them in favor of a better, kinder, wiser, more loyal significant other than any of them could ever be.
Even while learning how to connect more deeply with their therapists, trauma sufferers in particular may never learn how to engage in the daily give and take of real-life relationships beyond the therapeutic cloister. It’s no wonder our fabulous techniques don’t always stick and our clients still feel isolated, helpless, and unable to function back in the real world. Of course, good, responsible, hardworking therapists then blame themselves, thinking maybe they need to get more training, meditate harder, or go into therapy themselves. But here’s the real problem: no matter how much we help our individual clients better understand themselves, recognize their own stumbling blocks, and use new skills to rebuild themselves from the inside out, we haven’t woven change into the fabric of their daily lives, the ones they share with people who aren’t their therapists.
Bringing the Outside In
Clients, especially those who’ve been traumatized, often feel disconnected from themselves and somehow separate and cut off from other people, including members of their own families. Unfortunately, our one-on-one approach to treating them perpetuates this experience of being “other” in their daily lives—being the victim, the sick one, the outsider who’s not understood, validated, or welcomed, even in his or her own home. By implicitly emphasizing their separate and isolated status in therapy, we contribute to estranging them even more from the relationships that mean the most to them.
In Steve’s case, I inadvertently contributed to, and even strengthened, this dynamic. I became the loving companion he was missing, and for me, his wife became the demeaned other to blame, creating a toxic therapeutic triangle. Eventually, with help from my peer supervision group, I realized that we were spinning our wheels in therapy, and I finally told Steve that I couldn’t continue our work together without meeting his wife. I don’t know what exactly I was expecting Carol to be like—a gorgon with snakes for hair? a screeching harridan?—but the real woman was quite a surprise to me: from the moment she opened the waiting-room door, she showed that, although nervous, she was glad to be there.
Without hesitation, she told me right away why she was upset with Steve and, in fact, with me. “After he comes back from seeing you,” she said, “he just seems so remote. He won’t even look at me and hardly says a word. I think therapy has helped him be less anxious, but it hasn’t changed how he avoids me. Sometimes, I get the feeling he really wishes he could just leave us. I know he thinks I badger him, but I’m so scared he’ll really go. I couldn’t stand that a second time.”
As is often the case with the spouses of traumatized clients, Carol had her own trauma history. Her mother had left her family when Carol was eight years old. It was clear that Steve’s individual therapy not only increased her sense of insecurity with him, but triggered her terror of being abandoned for the second time by a person she loved. From the family therapy perspective, we’re always skating on thin ice when we fail to include the key players in the client’s life—the people who help them feel safe and secure or, conversely, make them feel insecure and threatened. Often, of course, these are all the same people.
So what are the concrete clinical advantages of taking a more systemic approach to the treatment of trauma? When the relationships of our clients are enacted right in front of us, we have a much more realistic view of what’s happening at home, what’s triggering their traumatic symptoms, and what’s helping or hurting their ability to function. With a systems approach, we’re not just hearing stories about people, but actually experiencing them ourselves, feeling in our own bodies what happens between people and seeing the patterns acted out.
I explained this to Carol in several individual sessions with her, and, along with Steve, we determined that they’d work together in couples therapy with me. Early on, I watched Steve shut down, roll his eyes, avoid topics, change subjects, and basically block Carol out as she tried with increasing desperation to get and keep his attention. After a minute or two of this, her face began to contort with bitterness as her voice grew shrill. “I know why you won’t talk to me,” she hissed, “You can’t talk to anybody. You don’t trust anybody because you’re a narcissist. All you think about is yourself.”
Steve turned his whole upper body away from this barrage, but gave me a quick, disgusted glance as if to say, “See what I have to put up with? Would you want to be married to this?”
There it all was, in living color: she tries to connect, he turns away. She feels rejected, tries harder, and he grows even stonier. She blasts him with cruel, sarcastic jabs, and he withdraws completely. In one session—actually, in one five-minute segment of one session—I was able to glean more valuable information about Steve’s life at home than I was after months of working with him individually.
My subsequent work with Carol and Steve illustrates how what at first may seem like baby steps can lead to big changes. During one session, Carol spontaneously began laughing at Steve’s imitation of his grandfather’s Italian accent. “Maybe if I spoke Italian more, you’d like me better,” he said to her. That led to a discussion of how Carol’s high-wattage smile had always melted Steve’s heart. Thus, we developed an agreement about how Steve could warn her of the onset of one of his dark moods by channeling his Italian grandfather, at which point she’d remember the uplifting effect of her smile. As they developed the ability to shift each other’s moods and connect more lightheartedly, they introduced new awareness into their relationship.
In my experience, these moments of finding safety and connection in the beginning of family and couples work are necessary to do the deeper work of understanding how terrible events in their past lives affect their lives today. Helping family members rediscover some of what they like and love about each other is a necessary preliminary to their being able to share their underlying pain and deeply troubled history with each other. To create the safety that will allow clients to be more vulnerable and less defensive, family members need to develop some of the qualities that we therapists try to cultivate in ourselves. Instead of separating clients from their families, our task is to encourage healing partnerships within families, allowing them to support each other in the process of healing, rather than relying exclusively on the therapist as the primary agent of change.
With Steve and Carol, we stayed focused on their mutual goals, how they truly wanted the same things for each other and their family. Armed with a new awareness of safety and humor in their relationship, they had many repeated experiences of valuing each other and feeling more empowered in the marriage and less afraid of one another, both inside and outside the consulting room. We could then venture into the stormy waters of Steve’s use of porn and Internet gambling to cope with his anxieties. Yes, I’d spent many previous individual sessions discussing this issue with Steve—but with Carol in the room, we could tackle how her own moods and demeanor often sent him flying to the computer in the basement, and how she herself could better deal with her own anxieties, stemming from her own history and experience with trauma. Soon, she learned some of the dialectical behavior therapy skills that Steve had picked up from his own therapy, and, instead of being threatened by them, she discovered how to support his use of them. For his part, Steve learned to take breaks from her in a way that wasn’t threatening to her and didn’t involve porn or gambling, and instead of fearing her intensity, he began to see it as an expression of her energy and passion. Over time, his anxiety subsided, as did Carol’s. They learned how to use their self-regulating skills to reinforce change in each other, even without me around—the once polarizing but now genuinely unifying therapeutic figure in their lives.
Bearing Witness
Another benefit of involving family members in trauma treatment is that, as therapists, we get the opportunity to bear witness with compassion and empathy to what our clients and their families actually experience, not just what they tell us they experience. This is a deeply validating experience for both the trauma survivor and other family members, who often feel dismissed, blamed, and isolated in their own suffering. Telling families that we see and recognize how what one family member says or does hurts or frustrates another has a deeply healing impact. Perhaps even more powerful is the opportunity to reinforce and confirm positive changes of behavior and interactions right then and there. Of course, this is a staple of most good individual work, but it has a multiplying effect with an entire family.
Mira, for example, had been severely sexually abused as a child. At age 47, she’d been in therapy, both group and individual, for many years. Because she felt safe with her therapist and worked hard in groups, she eventually became less anxious, stopped pulling out her hair and hitting herself, and began to connect with the others in group therapy. But the rest of her life remained a mess. She couldn’t keep a job because she fought with coworkers; and at home, she and her husband of 25 years regularly screamed, hit each other, and threw things until she’d retreat to her bed with a bottle of booze, sometimes for days.
Her 16-year-old daughter, Hannah, wasn’t doing well either. She skipped school as much as possible to get stoned and drunk with her friends, and when she came home, she contributed to the family melodrama by yelling and throwing things as well.
Week after week, Mira complained about her family, insisting they were the cause of all her problems. Thus, since Mira’s progress was clearly stalled, her therapist referred her to me for family therapy, and it was a tattered little group I met at that first session. The family was obviously not enthusiastic about coming. They’d seen little change in Mira after all her years in treatment and were convinced that therapy was a waste of time and money. Furthermore, they’d come to regard therapy as the place Mira came to be told what a noble, suffering person she was, and how badly her obnoxious family was treating her.
“We know you think we’re the problem,” said Mira’s husband, Fred.
“Yeah,” echoed Hannah, “so she gets a free pass to be as nasty as she wants at home.”
In spite of this rough beginning, when I explained to them that therapy was a way to help each person in the family feel better, not just Mira, they began listening with some interest. When I asked them about their goals for themselves and for the family as a whole, Hannah said she wanted her parents to stop yelling at her and leave her alone. Fred wanted to be able to put in a full day’s work without being called home to some emergency, usually involving his truant daughter and despondent wife, and not to feel angry so much of the time. And Mira, for her part, wanted to stop hating herself, feel that her family thought she was worth something, and “have some peace and quiet at home so maybe Hannah will spend more time there and do her homework.” In just those few minutes of calmly focusing on their common desires as both individuals and family members, they experienced a more sustained feeling of mutuality and togetherness than they had in years.
Now it was time for another powerful togetherness tool, what I’ve come to call Barrett’s Neuro 101. With charts and diagrams, I helped them understand how negative interactional cycles within the family trigger the emotional centers of every family member’s brain into a state of fight, flight, or freeze. In other words, each small, negative interaction is interpreted by everyone else as a high-danger alert, causing their nervous systems instantly to take action to ward off the threat by hitting and screaming (fight), bolting out the door (flight), or going into dissociative withdrawal (freeze). Some clients may be aware of how their sympathetic nervous system affects their own reactions, but most have no idea how closely knit together their family members’ systems are. Instead of hive brain, I told them, they share a hive nervous system—and it affects each of their day-to-day lives.
To help them understand further how negative remarks by one member of the family have a way of cascading into a torrent of painful interactions and symptoms, I recounted an incident they’d told me about earlier. When Fred had said something demeaning to Mira like, “It’d be a miracle if you could ever get dinner ready on time,” Mira’s fight response—easily triggered by any negative remark because of an already conditioned sense of fear and rage—kicked in. So she screamed, “Why don’t you try doing something around the house for a change, you jerk!” This caused Fred—now awash in his own fight response—to shout back, which caused Hannah—conditioned to react with instantaneous fear and anger to the volatility of the family—to run out of the house while Fred yelled after her, “Come back here right now!” Then Mira shrieked at her husband, “Look at what you’ve done!” and dissolved into a pool of tears and helplessness. Fred, thoroughly defeated, stomped out of the house, got in the car, and roared off.
Although Mira had described this type of scene to her therapist many times—and it was good therapeutic fodder for processing—it certainly didn’t prevent the scenario from repeatedly happening back home. But showing the whole family how these reactive feedback loops actually work, and how each family member contributes to them, is a powerful tool for getting them all to take responsibility for what really are their common problems, not just Mira’s. The goal, of course, isn’t to provide a one-time, cure-all dose of neuroscience nirvana, but to offer a clear structure of psychoeducational information that families can integrate into their emotional functioning, even in the heat of conflict.
One day, for example, several months into their therapy with me, Mira, Fred, and Hannah were in a crisis. Late the previous night, Hannah had left the house and didn’t answer her cellphone when Fred called to ask where she’d gone. After driving around and looking for her for hours, her parents found her at a park, high and drunk with her friends. They grabbed her, brought her home, locked her in her room, didn’t let her go to school, and then dragged her to therapy that afternoon.
In my office, Mira wailed, “I thought things were changing, but everything is just right back where we started.” Her face was pale and her body was trembling as she wiped furious tears from her cheeks.
As if picking up Mira’s upset like a fast-acting virus, Fred opened fire on Hannah, screaming, “Look what you’re doing to your mother! You’re going to kill her, and you’re going to kill yourself if you keep doing such damn stupid things!” As he yelled, he became red and started shaking his fists. I asked him to stop, sit, and breathe with me—to “pause and ponder,” as we’d practiced many times—but he bounded from his chair and moved toward his daughter, a look of pure rage on his face. There was no question that he meant to hit her.
In the old days of family therapy, I might’ve jumped up and blocked him with my body, demanding that he sit down immediately. But years of working with volatile families had taught me the value of doing the unexpected at critical points in therapy. Plus, I didn’t want my voice tone, body language, or movements to threaten Fred, as that would further trigger his traumatic reactivity. And I didn’t want to make him feel powerless and devalued, as that would send the message that he was a common thug, incapable of changing his behavior. So I interrupted Fred’s meltdown by standing up, summoning as much calm as I could muster, and saying, “Fred, I’m really thirsty. All this yelling has dried out my throat. Let’s you and I go together to get a drink of water.”
Startled, but not feeling attacked, he turned and came with me. As we walked to the water cooler, Fred turned to me and said, “Thanks. I know what you’re doing.” Using what he’d learned in our previous sessions, he continued, “You got me out of my lower brain because I was in fight mode, and you wanted to engage my middle and upper brain. Okay, now that you’ve distracted me, we can figure out another way for me to deal with Hannah.” Fred paused. “See, I’m not so dumb,” he said, managing a small smile. “I’m ready to go back in.”
And Fred came through like a champ! He apologized and told his daughter that behind his anger was great fear that something would happen to her. Together, they forged a reasonable behavioral contract, discussing what time she’d be home at night, how she’d check in over the course of the evening, why they wouldn’t let her drive the car for the time being, and what things she could do over time to get the keys back.
As all this unfolded, Mira gazed at Fred with wonder and relief. Over the next few months, she smiled often at her husband and daughter, gave them loving taps on their knees in the midst of conversations, and heart-to-heart hugs as sessions closed. Of course, this family’s work was far from done, but this session was something of a small miracle. The crisis that occurred with Hannah had allowed something to happen that could never have taken place in Mira’s individual therapy. Not only had we all witnessed the cycle of emotional and verbal abuse and the threat of physical violence, but we’d had the priceless advantage of seeing how the cycle could be stopped mid-spin. The family could then begin consciously practicing different kinds of interactions and together reap the rewards of a genuinely changed way of living.
Of course, systems approaches to trauma treatment don’t always lead to moving family reconciliations. In fact, the result can sometimes be quite the opposite, as was the case with Melinda, who’d spent 10 years in therapy trying to come to grips with her mother’s neglect. While Melinda had certainly become a far more emotionally healthy person than when she began treatment, she was still haunted by the reality that her mother hadn’t been there for her as a helpless child. Often, while her mother was working nights or out drinking with friends, she’d been left alone with her mother’s boyfriends, several of whom had sexually abused her.
When Melinda had first started therapy with me, I told her that I like to include family members and even the friends of clients in sessions. We agreed then that there’d be a time when her mother would come with her to therapy, and we planned for Melinda to approach her mother with an attitude of curiosity, rather than a need to settle old scores.
When that time came, Melinda’s mother was restrained, clearly holding herself together for the attack she expected. Instead, Melinda calmly asked her questions about their life together and told her about her experiences growing up—without anger, without blame, but with real sadness in her voice. Hearing Melinda’s words, her mother began crying. “I know that I was never there for you,” she sobbed. “I was just working so hard to support you after your father left. I felt so completely depressed and just didn’t have anything left to give you. I’m sorry that I brought men in the house. I thought they’d take care of us, but they wound up hurting us both.”
Soon, however, as the conversation continued, her mother’s demeanor changed. A wall came down as she switched tones and angrily lashed out at her daughter for holding on to old grievances. “You’re grown up now!” she yelled. “You’ve done fine in life! You didn’t have it nearly as hard as I did with my rotten excuse for a mother! Why are you still having a pity party for yourself because of something I did or didn’t do decades ago?!”
Rather than being crushed by yet another experience of parental harshness and abuse, as I initially feared, Melinda wound up feeling deeply empowered by this session. The next week, she told me that having me witness her mother both validate and invalidate her as a person within 30 minutes had affected her more positively than all of her other therapy put together. Therapist after therapist had told her to give up on wanting anything from her mother, to let go and grieve the loss, which she simply couldn’t do. But now that I’d seen and heard her mother in person, Melinda felt at peace. She no longer wondered if what she’d experienced had been true. At last, she really could stop knocking repeatedly on the same door and realize that the mother she wanted simply didn’t live there. It was time to move on.
Healing Partnerships
So why are trauma therapists so often hesitant to integrate family and couples approaches into their work? Why, more often than not, do they choose the safe haven of individual therapy, even when it has limited impact on interrupting and changing the negative interactional cycles that keep both trauma survivors and their families retraumatizing each other? Mostly, I think we avoid families because they can be so exhausting, creating an atmosphere of great emotional volatility, which requires us to be on our toes all the time. But beyond the inconveniences and emotional challenges of systems approaches, I believe the overriding reason that they’re not used more is that our professional training doesn’t encourage us to expand our vision of our clients’ lives and their pathways to healing beyond their individual selves. In addition, too many of us naively accept our clients’ limited versions of the other people in their lives, or we listen to the opinions of referring sources, blind to family members’ strengths, as well as their failings. Creating healing partnerships among the people our clients interact with every day can’t be done in individual therapy. Nor can it be done at home, since it takes a safe environment to recognize destructive cycles and discover ways to interrupt them. This is especially true with trauma survivors. As they share their deepest feelings and narratives, they’re emotionally held not only by the therapist, but by the people who are most important in their lives.
Of course, Mira, Fred, Hannah, Steve, Carol—all my clients—will still experience disappointment, frustration, and anger, both individually and as families. But the more experience they have of working through their difficulties together—and understanding the impact of their behavior on one another—the less hopeless and the more empowered they’ll feel. Rather than any single magical technique or sage intervention, it’s repetition of positive experience that’s the true engine of change.
The therapy experience takes on an entirely different dimension when family members learn to be healing agents for each other. As Carl Whitaker once asked, “Who would you rather get a hug from, your mother—at least after she realized the meaning of a real hug—or your therapist?”
Illustration © Dave Cutler
Mary Jo Barrett
Mary Jo Barrett, MSW, is the founder and director of Contextual Change and coauthor of Treating Complex Trauma: A Relational Blueprint for Collaboration and Change and The Systemic Treatment of Incest.