If post hoc diagnosis is any indicator, many of history’s most illustrious figures had some version of what we now call obsessive compulsive disorder (OCD), including Thomas Jefferson, Ludwig van Beethoven, Charles Darwin, Marcel Proust, Sir Winston Churchill, and Albert Einstein. Apple cofounder Steve Jobs even got down on his hands and knees to search for specks of dust on the floor during the rollout of the first Mac computer.
Certainly, in our time, many habits of mind associated with workplace success—single-minded dedication, concentration, persistence, intensity—might appear to have a certain OCD-ish quality. But anybody who’s truly experienced the real OCD, or known someone who suffers from it, realizes just how nightmarish the actual condition can be. It turns people into prisoners of their own minds, locked into an ever-shrinking cell of unwanted mental preoccupations and the frantic desire to escape them—which has the paradoxical impact of strengthening them, thus reinforcing the whole miserable cycle.
Although I didn’t know it as a child—nor did anybody in my family—my mother, it now seems clear, suffered from OCD. Among her symptoms was a preoccupation with the idea, after she’d spoken with someone on the phone, that she’d said the wrong thing, which necessitated a compulsive need to call the person back, to explain, to apologize, to make it all right. This, of course, only sank her more deeply into the quicksand, intensifying the unshakeable conviction that she’d somehow offended the person again, needed to make amends again, must call again to repair the fault committed during the last call—and on and on and on. No one in my family had ever heard the term obsessive compulsive disorder back then. To us, this behavior was just one more of my unhappy mother’s incomprehensible nervous tics.
So today, with all the presumed advances therapists have made in reducing mental suffering from previously untreatable conditions, is there a solution, a cure, a fix for OCD? As with so many difficult emotional conditions, the answer is far from simple, not least because, like bipolar disorder and schizophrenia, OCD appears to bear a strong genetic component. Still, we have more knowledge about how to recognize it, and how to distinguish it from other conditions that it often mimics, including PTSD, depression, and even psychosis. More importantly, many specialists working with OCD employ some variation on what two authors for this issue, Martin Seif and Sally Winston, call “upside-down therapy,” an approach that seems to break, or at least bend, the rules of what many of us have been taught is good clinical practice.
The hallmark of their method is to resist the temptation to explore the often bizarre content of the client’s obsessions or teach the client skills to refute them cognitively. What’s needed instead, according to Seif and Winston, is a more paradoxical approach, which reduces the “sticky mind” of OCD by helping clients develop a different kind of relationship to their inner preoccupations, a relationship that looks quite a lot like an inspired form of benign neglect. Indeed, while always supportive of the client, the successful OCD therapist, in effect, offers no support whatsoever for the obsession. It’s more complicated, of course, than saying, “Ignore it and it’ll go away.” But Seif and Winston insist that a form of mental starvation of the symptom does seem to make it quieter and less intrusive. We may not yet have the clinical tools to make OCD disappear entirely, but we’ve learned a thing or two about how to make it a more docile beast.
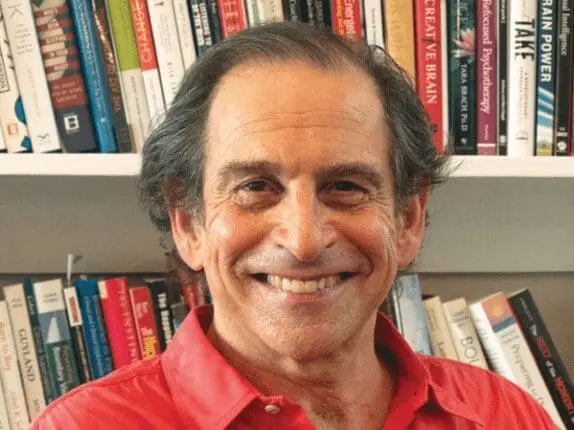
Richard Simon
EDITOR
Rich Simon
Richard Simon, PhD, founded Psychotherapy Networker and served as the editor for more than 40 years. He received every major magazine industry honor, including the National Magazine Award. Rich passed away November 2020, and we honor his memory and contributions to the field every day.