Quandary: One of my clients takes prescription medication for anxiety and often complains about the negative side effects. I can’t help but feel it’s getting in the way of his treatment, but I hesitate to suggest he get off the medication since I’m not an expert in this area. What should I do?
1) Let the Client Choose Their Own Adventure
Being a caring therapist sometimes feels like you’re in a “Choose Your Own Adventure!” story. You know you want to have the “right” impact on your client, but what does that mean? What if you make a Bad Choice?
“You tell your client he should stop his meds. Go to page 46 if your client stops and then blames you for ruining his life. Go to page 5 if your client stops and blesses you for being the best therapist ever. Go to page 22 if your client keeps taking the meds but quits seeing you. Choose any page between 68-175 if your client ignores you and keeps doing what he usually does, though with some interesting twists and turns…”
Don’t go down the rabbit hole! Your client will always choose his own adventure, so be prepared to trust that (which can take some deep breaths on your part). That’s his challenge. Your challenge is to be an anchor your client can trust to help him see his choices more clearly.
How to do that?
Step One: Find your own story. Taking a few more deep breaths, ask yourself: what are you really worried about? You’re not happy with how treatment is going, so explore that. Are you feeling bored or impatient with your client? Are you doubting your skills as a counselor? Identify what’s really important for you to address—the underlying worry that you can then turn into a direction. You’re no longer trapped in trying to figure out what’s “right” for your client.
Step Two: Approach your client with honest appreciation for his strengths. You do this by truthfully flipping what you first thought was a problem into what you can now see as integrity. “You care deeply about handling your anxiety better. You’re so committed that you’re willing to cope with these unpleasant side effects from your meds. That’s impressive determination.” Let your client know you’re aligned with his goals while having compassion for his struggles. Be his anchor.
Step Three: Help your client explore his own choices. He is facing his “Choose Your Own Adventure” options, and he’s worried. What if he stops his meds and gets worse? What if he doesn’t stop and gets worse? What if he can’t afford his meds? What if he feels like a therapy failure? There are always what-ifs. Help him shift from the fear of making the wrong choice to having trust in his journey. Because it’s never about any one choice; it’s about reaffirming your client’s sense of growth.
Ken Fremont-Smith, LMHC, Certified Gottman Therapist
Seattle, Washington
2) Explore, Don’t Fix
When a client repeatedly brings up something in session, they want to talk about it with us. They want us to be curious about it. It’s not something for us to fix, but it is a way for us to help the client explore their feelings and thoughts about that particular concern.
While you may not be an expert in medication, you do have some expertise in observing and noting recurring patterns and themes that show up for clients. If your client is telling you explicitly that they’re experiencing negative effects from their medication, perhaps a good starting point is to reflect to them that they’ve mentioned this a number of times in session and ask them about it.
Are the negative effects outweighing the positives? Can you help them list the pros and cons of the medication? What was life like before they took this medication? What do the people close to them notice about the effects of the medication? Have they discussed the effects with their prescriber? Are there real or perceived obstacles to discussing the effects with him or her? Can you help role play a discussion with the prescriber? Are there ways of mitigating the negative effects, such as exercise and nutrition for weight gain, or mindfully connecting to their sexuality and sensuality for loss of libido, that you could discuss?
You could also have a call with the client’s prescriber to discuss the impacts of the medication and whether there are alternative ones. You could also discuss non-pharmaceutical treatments for anxiety with your client, such as Acceptance and Commitment Therapy, exercise, CBT, or reduction or abstinence from alcohol and caffeine, to give them options and agency in deciding what treatments they prefer. Obviously if they decide to stop using their prescribed medication, the tapering off process must be supervised by a doctor over an extended period of time. At this time, they can start, on a routine daily basis, to increase their use of the non-pharmaceutical treatment options, building a skill set they can rely on to manage living with the anxiety.
Siobhan Hannan, psychotherapist and counsellor
Sydney, Australia
3) A Manual in Plain Sight
Where’s the best manual to treat your client? Remember, it’s right in front of you—it’s the client! How do they feel about taking the medication? Is there someone in their life who’s against them being on medication? If they don’t believe in taking medication, cognitive dissonance may be at work. If someone significant in their life is against them being on medication, the fear of becoming disconnected from that person could also be creating internal conflict.
Do they believe the medication is working and that they need it? There are many medications in the world, but not all of them work on everyone with the same results. Is the medication prescribed by an MD or a psychiatrist? Some physical issues, such as thyroid issues, can affect our life balance, including our emotions. I once had a client who had been prescribed Klonopin by his MD because of anxiety and stress issues. Several months later, he had another MD in the emergency room look at his blood work and diagnose him with Chron’s disease. After slowly getting off the Klonopin and getting treatment for his Chron’s, his life was much better. So, give this client a referral! When’s the last time they had a physical exam to check if there’s something else out of balance, physically speaking, that needs to be treated? Have them check with their provider for an alternative anxiety medication that may work better for them and possibly alleviate the negative symptoms being experienced.
You’re not alone in this, and giving your client the right referral and helping them get the right treatment can make a world of difference in their outcome.
David Ian Copeland, PhD, LMHC-S
4) Listen, Investigate, Explore, Consult, and Empower
Disclaimer: like this therapist, I also don’t consider myself an expert on this subject—so we’re in good company!
I think the most important thing to do is to listen to the person sitting right in front of you before moving to action. This client is complaining about negative side effects, so listening to those feelings would be my first decision. I’d try to understand as best as I could what the client is going through, even though I wouldn’t be experiencing what they were. I would create a list of pros and cons of the medication. I’d also want to gauge if the negative side effects of the medication outweigh its benefits. One of the hardest things for me to do in therapy (and life in general, honestly) is to not jump to solutions, because I want to help so badly. Social work teaches me to empower the people I work with, recognizing them as the masters of their own ships and the experts of their own lives. We are lending them our eyes, ears, heart, compassion, and space to come to their own conclusions about what is best for them.
So, the short of it is this: listen, investigate, explore, consult, and empower. Listen to what they have to say and how the experience has been. Investigate the side effects to the medication (what are they, when did they start, how often do they occur, how severe are they, etc.). Explore by weighing the side effects against the effectiveness of the medication. Is the anxiety lessened with the medication or have the side effects caused more anxiety or discomfort? Consult with the prescribing provider about what you’ve learned—a team huddle, of sorts—while recognizing the most important member of the team is the client. Last, empower the client to make a decision, and put the ball in their court as to how they’d like to move forward given the options, such as looking at different medications or changing dosages or the time or method the medication is taken.
Ja’Lise Brown
5) Collaborate, but with Limits
Every now and then we therapists may experience concerns about protecting our clients. We try to do our best for their well-being. But sometimes, in trying to protect them, we increase the possibility of violating boundaries. We may prevent the client from taking responsibility for themselves, or we may mislead them consulting about an issue that’s not our specialty. In such cases, we’re more likely to harm the client than help them.
During the therapy process, many factors may arise that affect our clients’ well-being. They can be caused by the client, the therapist, therapy itself, or the many variables that affect the client outside of therapy. In this case, one of these variables is the client’s prescription medication. Personally, I think that the client’s use of medication is best left to the prescribing doctor and the client. The client’s decision to take medication shouldn’t depend on what their therapist thinks.
On the other hand, if we observe something wrong with our clients, it’s unprofessional to be indifferent. Isn’t it also the duty of therapists to help clients improve their quality of life? In this situation, I think it would be appropriate to bring this up with the client in therapy. They can talk about how the medication affects them, and their motivation (or lack of motivation) to continue using it. If the client decides to stop using medication, you can also discuss how his life may change.
It’s important to note that the client has another, separate process with the prescribing doctor. I believe therapists should be involved in this process. This way, we can discuss with prescribers problems that medication may cause and share our observations. I’d advise this therapist not to worry: it’s clear that your intention here is to demonstrate your care for your client, not that you’re trying to step outside of your role. Ultimately, it’s up to the client to decide whether to continue using medication, but better understanding our own role—and our limits—is best for both client and therapist.
Alper Karababa, systemic therapist and counselor
Mugla, Turkey
Photo © iStock/nadia bormotova
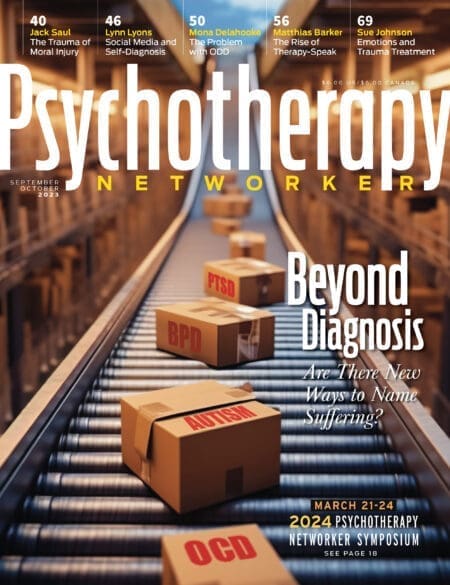
Psychotherapy Networker
The editorial staff of Psychotherapy Networker comprises clinicians, journalists, and writers with a passion for creating a community where therapists gather and grow. Learn more on our About Us page.